For most, the idea that you might don a headset to zap your depression away or use electromagnetic pulses to sharpen your cognition seems better placed in a science fiction novel from the 1930s than modern neuroscience, but these kinds of treatments are more common than you might think.
In fact, you can now buy “vagal reset” gadgets to practice what’s broadly referred to as neurostimulation at home – Instagram and Tiktok are awash with ads for them. And for more intense forms of this kind of technology, a quick online search will deliver a range of private clinics offering “repetitive transcranial magnetic stimulation” to treat depression and anxiety.
Tennis legend Serena Williams is among those who’ve checked into a private facility to undergo a treatment like this. The athlete recently shared a sponsored Instagram post about her “ExoMind” journey, describing the treatment as a form of self care. Williams’ caption in the ad post read: “I never do enough self care and my friend introduced me to @exomindbtl and it’s really changed how I’ve prioritized wellness, not only for my muscles with @emsculptneo, but also for my mind.”
The company responsible for ExoMind describes the treatment as “a workout for your mind. An FDA-cleared for the treatment of depression”. The company also offers treatments that use electric pulses to tone and strengthen muscles all over the body – from the stomach to the pelvic floor.
But naturally, Williams’ Instagram post prompted some confusion about possible uses for neurostimulation, delivery methods and who should be using technology like this. Do we need to be nudging our brains with electrical stimuli for improved “mental fitness”? Or should we just stick with mindfulness apps and fish oil supplements for better brain health?
Furthermore, is neurostimulation actually a serious cure for depression? Do you need to visit a clinic or will an at-home headset deliver the same results? And most importantly, is this all safe?
What is neurostimulation?
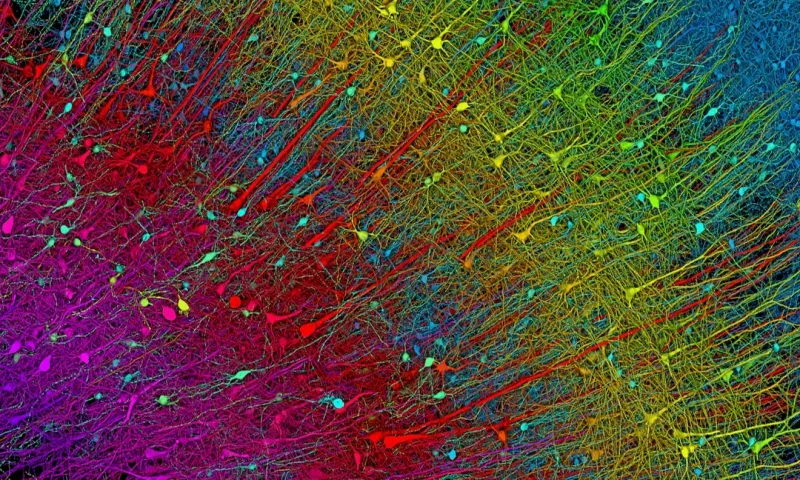
Neurostimulation is the act of stimulating the brain, spinal cord or peripheral nerves to modulate neuronal activity. There are a variety of ways to do this and types of neurostimulation vary. For example, a headset that you can buy online without a prescription that promises to “reset your vagus nerve” is not the same as an in-clinic transcranial stimulation session delivered by a qualified practitioner.
The Flow headset, for example, sends the equivalent current of an AA battery directly to the dorsolateral prefrontal cortex, “targeting depression at its source to help relieve symptoms”. Rival company Neurosym claims that its device emits precise electrical pulses for “safe stimulation of vagus nerve fibres”. The company isn’t clear on how this approach differs from Flow’s, but it does claim that the device activates the parasympathetic nervous system to “effectively manage chronic pain, fibromyalgia, gut problems, long-covid symptoms, inflammation, POTS symptoms, fatigue, sleep issues, HRV issues, ADHD symptoms, stress, anxious and depressive thoughts and more”. Quite the list of claims.
Pulsetto, another headset that you can use at home, also describes itself as a “vagus stimulator”. Pulsetto technology uses the lowest form of bluetooth energy – ultra low radiofrequency energy (ULRE) – which according to the brand, “passes safely into the body to biohack your parasympathetic nervous system”.
“These headsets have great branding but in reality you don’t know the exact effects that treatment is going to have on you,” says Adam O’Hagan, specialist rTMS practitioner and coordinator at Priory Wellbeing Centre Harley Street.
“The do-it-yourself kits have shown to be effective but not as much as in controlled settings. Some headsets use rTMS in low levels but they’re very different to what we do. They can be more cost effective but use different technologies and these can be significantly less effective.”
The kind of treatment offered at Priory differs vastly from headsets like Flow and Neurosym – technologies that you can easily buy online albeit for a high price point. Technically, all treatments fall under the umbrella of neurostimulation, but there are significant differences when it comes to the technology and frequencies used, and the applications and results.
The idea with both in-clinic treatments and do-it-yourself headsets is to nudge the areas of the brain that are responsible for emotional regulation, cognitive function and self-control. These areas can often become under-active and this lack of activity is associated with low mood, anxiety, depression and behavioural disorders. Neurostimulation devices generate magnetic pulses to induce electrical currents in the brain, stimulating under-active brain regions.
“An in-clinic session can last about 30 minutes and is typically recommended for treatment-resistant depression, obsessive compulsive disorder, significant eating disorders and anxiety symptoms. The intensity of the machine used is much higher and the treatment is administered by a trained professional,” explains O’Hagan.
“During an rTMS session, electromagnetic coils are placed on your scalp in order to deliver magnetic pulses to your brain. The treatment specifically targets areas of the brain that are involved in mood control, which means it can help to alleviate the symptoms of your mental health conditions and improve wellbeing.”
“The side effects are extremely minimal compared to other treatments such as medication, so it’s a much safer and less invasive solution. Some patients can see results after five sessions or around the halfway mark in the treatment plan,” he adds.
It’s worth noting that rTMS is very different to electroconvulsive therapy, or ECT, which sends a seizure-inducing current through the brain. Doctors have used ECT for almost a century, and though it’s still used in some cases, it remains a controversial and rudimentary treatment.
Mental fitness and biohacking the vagus nerve
At the other end of the neurostimulation spectrum are home devices – headsets that deliver a mild electrical current to the brain and that can be worn daily on the head or neck. These devices offer “improved mental fitness” – a catch-all term that seems to comprise several indicators of good health such as boosted mood, lower anxiety levels, improved memory and cognition, and better focus.
The biohacking and longevity crowd are especially keen on the idea of fitness for your mind – Bryan Johnson wears a Pulsetto headset in his Netflix documentary Don’t Die. However, Dr Faye Begeti, practising neurology doctor at Oxford University Hospitals and author of The Phone Fix, explains that the term mental fitness is actually quite vague if we’re discussing the true benefits of these devices.
“The term ‘mental fitness’ allows companies to market these devices without clear scientific backing,” she says. “While some biohackers report subjective benefits, scientific evidence supporting any substantial long term improvement from these devices is weak.
“Established good brain habits such as adequate sleep, regular exercise, learning new skills to build cognitive reserve, and stress management have stronger evidence for improving brain function over time. Expecting dramatic improvements in memory, focus, or productivity from neurostimulation devices is likely unrealistic.”
But as mental health issues such as anxiety and depression continue to affect large swathes of the UK population, people are looking for alternative sources of support – particularly within biohacking and functional medicine. So despite scant evidence that at-home devices can help – and their hefty price tags – neurostimulation headsets have become incredibly popular.
This might have something to do with the fact that social media is currently flooded with instructional videos on “how to reset your vagus nerve”. These techniques range from simple massage and acupressure to recommendations for headsets like the Neurosym or Pulsetto.
“The vagus nerve ‘reset’ trend is a mix of science and misinformation,” explains Dr Begeti. The vagus nerve plays a key role in the parasympathetic nervous system, which helps regulate stress, digestion and heart rate. Activities like spending time in nature, meditation, and breathing exercises can stimulate vagal tone, which may have calming effects – but calling it a ‘reset’ or a ‘detox’ is misleading. The nervous system is not something that needs ‘resetting’ in the way social media often suggests.”
“The issue is that social media often oversimplifies complex neuroscience, making it seem like a single technique is a quick hack for mental health. Instead, it’s important to have multiple tools in your toolkit for managing difficult emotions while also seeking professional advice when needed,” she adds.
The verdict
As Dr Begeti says, there’s no one trick to eliminate mental health issues. A healthy diet of gut-friendly foods, regular exercise, quality sleep and other techniques like breathwork, yoga and time in nature can all have a positive impact on the brain and nervous system when combined. In isolation, a neurostimulation device won’t make much difference if you’re not taking good care of yourself.
However, the most recent studies on the effects of clinical rTMS are promising. “We are witnessing a growing mental health crisis,” explains O’Hagan. “Depression is treatable, but for some people, medication and psychotherapy do not provide relief. In such cases, rTMS is a really incredible new tool.”
The important thing is not to downplay the intensity of a treatment like this. Though it’s akin to tickling your brain, one should be aware of the risks. Various studies have shown that neurostimulation can help improve mood, but a small number of patients have experienced long term effects like tinnitus, cognitive impairment, behavioural changes and short term memory loss.
These outcomes are far less likely with an at-home treatment as the power generated by a wearable isn’t comparable to an in-clinic rTMS treatment. However, there are still risks associated with using one. You are, after all, giving your brain a buzz, regardless of the dose.
“The biggest concern is that many brands do not disclose the exact stimulation parameters, making it difficult to know what effect the device is actually having. Additionally, improper use – such as applying stimulation to the wrong area of the brain – could lead to unintended effects,” says Dr Begeti.
She advises researching the frequency and intensity used in detail and checking if the device has been tested in peer-reviewed studies, rather than relying on general research. She also recommends checking for FDA approval or CE certification for specific medical conditions, as opposed to general wellness claims, and reading the instructions thoroughly.
“For low mood, anxiety and issues with feeling dysregulated, a headset could help,” says O’Hagan. However, the best course of action is to use a wearable in conjunction with other healthy habits. These devices are definitely not a magic bullet and O’Hagan recommends using them alongside other interventions like talking therapy and daily self care routines.
“Typically I wouldn’t recommend them for people with clinical depression,” he says. But this is where a treatment like clinical rTMS might make a difference, particularly if you’ve tried other treatments and found them inconsistent or unhelpful.