Research by scientists at the University of Southern California (USC) Leonard Davis School of Gerontology suggests that greater exposure to extreme heat may accelerate biological aging in older adults.
The study, which examined the association between ambient outdoor heat and epigenetic aging in thousands of individuals aged 56 years and older, raises new concerns about how climate change and heat waves could affect long-term health and aging at the molecular level.
Research lead Jennifer Ailshire, PhD, professor of gerontology and sociology at the USC Leonard Davis School, said people in neighborhoods that experience more days of high heat show greater biological aging on average than residents of cooler regions.
Ailshire is senior author of the team’s published paper in Science Advances, titled “Ambient outdoor heat and accelerated epigenetic aging among older adults in the US,” in which the team concluded, “These findings provide insights into the biological underpinnings linking heat to aging-related morbidity and mortality risks.”
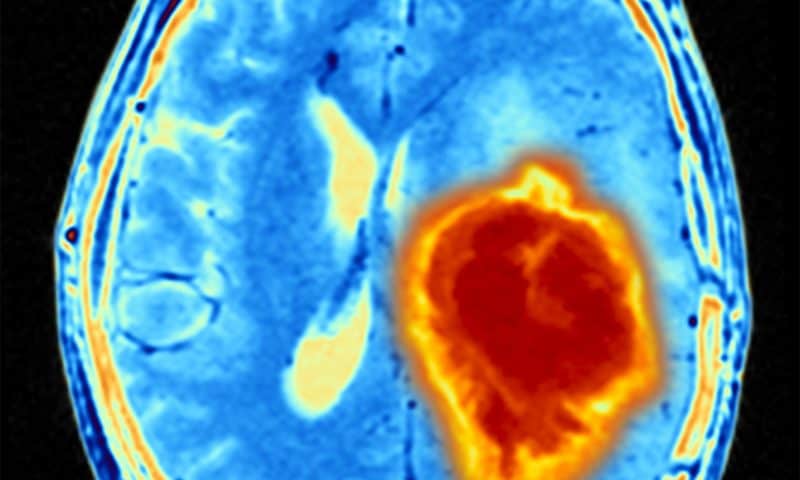
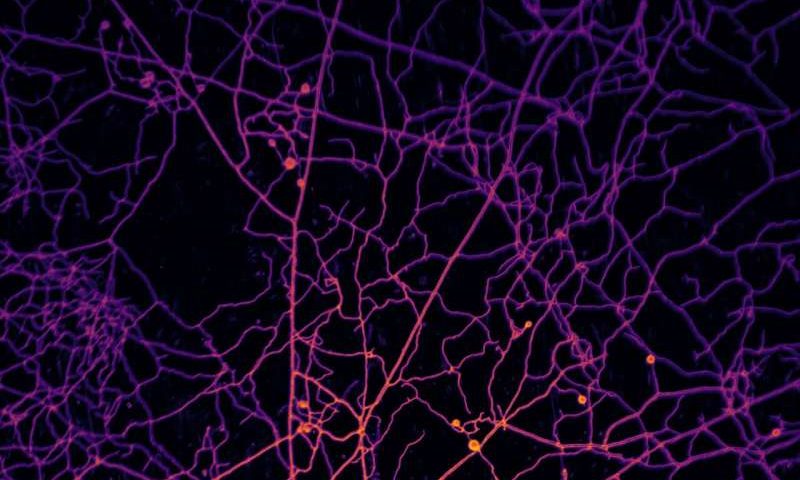
Biological age is a measure of how well the body functions at the molecular, cellular, and system levels, as opposed to chronological age based on one’s birthdate. Having a biological age greater than one’s chronological age is associated with higher risk for disease and mortality.
“Global warming has intensified extreme heat events, posing serious risks to public health,” the authors wrote. “The frequency, intensity, and duration of extreme heat events are expected to grow rapidly in the coming decades, affecting more than 100 million Americans in 2050.” Exposure to extreme heat has long been associated with negative health outcomes, including cardiovascular diseases, and an increased risk of death, but the link to biological aging isn’t well understood.
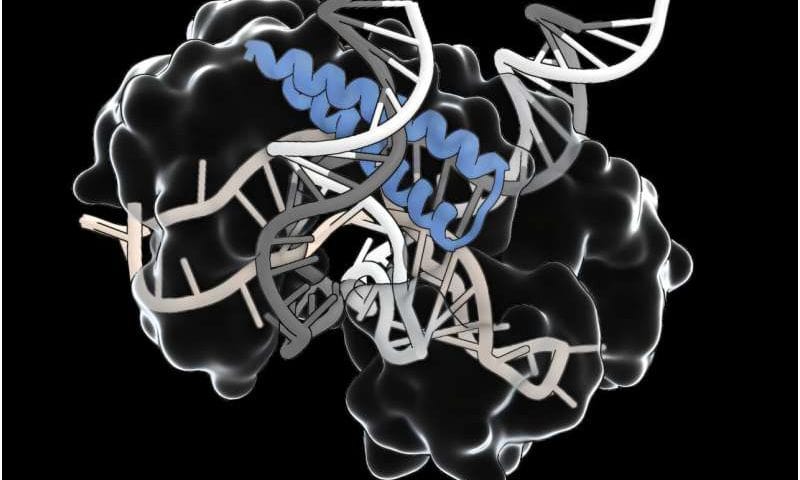
Ailshire and co-author Eunyoung Choi, PhD, USC Leonard Davis School of Gerontology alumna and postdoctoral scholar, examined how biological age changed in more than 3,600 Health and Retirement Study (HRS) participants aged 56 years and older from throughout the United States. Blood samples taken at various time points during the six-year study period were analyzed for epigenetic changes, or changes in the way individual genes are turned off or on by a process called DNA methylation (DNAm).
“This study examines the association between heat and epigenetic aging in a nationally representative, diverse sample of older adults,” they explained. The effects on the body of heat events may not manifest immediately as clinical conditions, the investigators continued. “Rather, these environmental insults may elicit subclinical deterioration at the biological level, accelerating biological aging, which precedes the subsequent development of diseases and disabilities.” And while the effects of heat on DNAm have been reported across a number of different species, including fish, chickens, and some mammals, there have been very few studies in humans. “Our study bridges this gap by examining epigenetic age (or clock), a molecular marker of biological aging based on DNAm levels throughout the genome.”
To carry out their study the researchers used mathematical tools called epigenetic clocks to analyze DNA methylation patterns and estimate biological ages at each time point. They then compared participants’ changes in biological age to their location’s heat index history and the number of heat days reported by the National Weather Service from 2010 to 2016.
The National Weather Service Heat Index Chart categorizes heat index values into three levels based on the potential risk of adverse health effects. The “Caution” level includes heat index values ranging from 80°F to 90°F, the “Extreme Caution” level includes values between 90°F and 103°F, and the “Danger” level includes values between 103°F and 124°F. Days in all three levels were included as heat days in the study.
The analysis revealed a significant correlation between neighborhoods with more days of extreme heat and individuals experiencing greater increases in biological age, Choi said. This correlation persisted even after controlling for socioeconomic and other demographic differences, as well as lifestyle factors such as physical activity, alcohol consumption, and smoking, she added. “Our findings reveal significant associations between more heat days and accelerated epigenetic aging, particularly for longer-term periods,” the authors stated.
“Participants living in areas where heat days, as defined as Extreme Caution or higher levels (≥90°F), occur half the year, such as Phoenix, Arizona, experienced up to 14 months of additional biological aging compared to those living in areas with fewer than 10 heat days per year,” Choi commented. “Even after controlling for several factors, we found this association. Just because you live in an area with more heat days, you’re aging faster biologically.”
All three epigenetic clocks employed in the study—PCPhenoAge, PCGrimAge, and DunedinPACE—revealed this association when analyzing epigenetic aging over a 1- to 6-year period. “We found consistent associations between long-term heat days and accelerated epigenetic aging across PCPhenoAge, PCGrimAge, and DunedinPACE,” the investigators noted. PCPhenoAge also showed the association after short (7 days) and medium (30–60 days) periods of time, indicating that heat-related epigenetic changes could happen relatively quickly, and some of them may accumulate over time. “Specifically, we observe that short-and mid-term heat conditions are significantly associated with increases in PCPhenoAge, while more heat days more than 1 year and 6 years are linked to accelerated epigenetic aging in all epigenetic clocks,” they added.
Older adults are particularly vulnerable to the effects of high heat, Ailshire said. She noted that the study used heat index, rather than just air temperature, to take relative humidity into account as they analyzed results.
“It’s really about the combination of heat and humidity, particularly for older adults, because older adults don’t sweat the same way. We start to lose our ability to have the skin-cooling effect that comes from that evaporation of sweat,” she explained. “If you’re in a high humidity place, you don’t get as much of that cooling effect. You have to look at your area’s temperature and your humidity to really understand what your risk might be.”
The next steps for the researchers will be to determine what other factors might make someone more vulnerable to heat-related biological aging and how it might connect to clinical outcomes. “Our study provides insights into the biological underpinnings linking heat to the broader spectrum of aging-related morbidity and mortality risks,” they wrote. “We demonstrated that short-, mid-, and long-term ambient outdoor heat can significantly accelerate epigenetic aging within a diverse, nationally representative cohort of older adults.”
In the meantime, the study results could also prompt policymakers, architects, and others to keep heat mitigation and age-friendly features in mind as they update cities’ infrastructure, from placing sidewalks and building bus stops with shade in mind to planting more trees and increasing urban green space, Ailshire said. The findings, the investigators noted in their report, provide “strong evidence critical for guiding public policy and advocacy initiatives aimed at developing mitigation strategies against climate change.”
Ailshire added, “If everywhere is getting warmer and the population is aging, and these people are vulnerable, then we need to get really a lot smarter about these mitigation strategies.”
The authors further concluded, “… our findings serve as a foundation for the development of targeted public health interventions, providing a strategic framework for addressing the adverse biological impacts triggered by extreme heat.”