The overall economic outlook for 2025 may show slow-but-steady growth—”above-potential GDP growth toward 2.2%,” according to EY—but the job forecast is more optimistic for the life sciences sector, which is expected to maintain record-high employment in 2025 after achieving an all time high of more than 2.1 million workers last October.
While employment growth in the pharmaceutical and medicine manufacturing subsector has stayed sluggish, that performance has been offset by record-high employment in the Biotechnology R&D subsector, commercial real estate firm CBRE found in its February 5 “U.S. Life Sciences Outlook 2025” report.
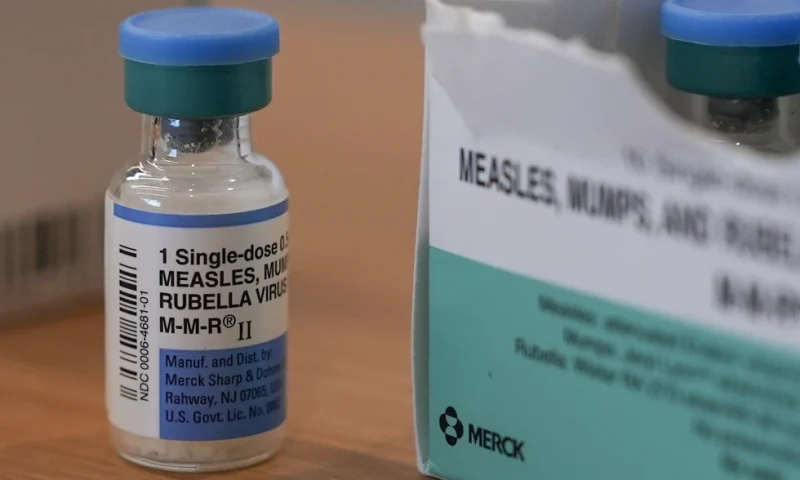
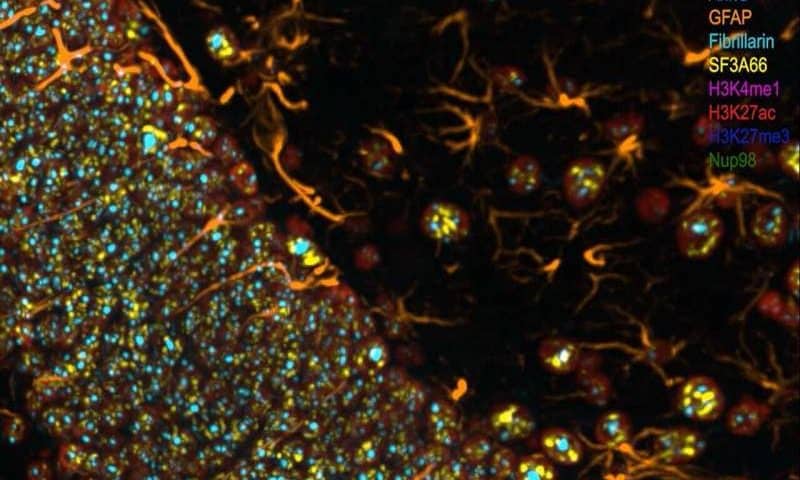
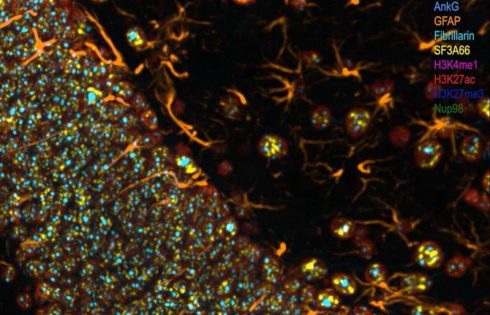
Between January and October 2024, Biotech R&D companies added 10,700 employees, for an increase of 3.7% that has propelled the subsector to a record workforce size of 303,000. Biotechnology R&D growth has been driven by advances in cell and gene therapy development, building on breakthroughs that had already yielded a jobs boom between 2012 and 2022.
This A-List contains 10 research and clinical biotech occupation categories projected to add jobs through 2033, according to the U.S. Bureau of Labor Statistics (BLS)’s Occupational Outlook Handbook, which was mostly updated last August, though additional information about biological technicians, epidemiologists, and medical scientists was added in December.
The occupation categories are ranked in order of the number of additional jobs that are expected to be created between 2023 and 2033.
Each occupational category is listed with BLS-calculated metrics that include the number of jobs in 2023, the percentage increase between 2023 and 2033, and the median pay per year in 2023. Accompanying these metrics is a BLS occupational description.
This year, as with GEN’s A-Lists of top biopharma jobs in demand published in 2024 as well as our 2023 A-List, the greatest number of projected jobs over the coming decade were for clinical laboratory technologists and technicians (also called medical laboratory scientists), i.e., professionals who collect samples and perform tests to analyze body fluids, tissue, and other substances.
Eight of the top 10 occupations highlighted in this A-List showed year-over-year increases in job openings projected over the next decade as compared with last year’s A-List—a clear improvement from last year, when 7 of the 10 occupations showed year-over-year declines in job openings. That appears to reflect increased hiring plans by life-sci employers across industry and academia despite ongoing concerns over the broader economy.
The largest drop in the employment change projected for 2023–2033 is among epidemiologists, whose projected number of jobs a decade from now was calculated by BLS at 2,100, down 22% from 2,700 last year. While no explanation was offered, one possible reason may be a reduced research emphasis on COVID-19 and future pandemics. Fortunately, epidemiology is the only occupation showing a projected one-year decrease. Genetic counselors showed the same number of projected jobs this year as last (600), and all other occupations showed increases ranging from 8% (clinical lab technologists) to 68% (chemical technicians).
1. linical Laboratory Technologists (Medical Laboratory Scientists) and Technicians
Projected employment change, 2023–2033: 18,200 more jobs
Job openings projected each year on average, 2023–2033: 24,200
Number of jobs, 2023: 344,200
Job outlook, 2023–2033: 5% (Faster than average)
Median pay, 2023: $60,780/year
About the position: Clinical laboratory technologists (also known as medical laboratory technologists) and clinical laboratory technicians (also known as medical laboratory technicians) perform medical laboratory tests for diagnosis, treatment, and prevention.
2. Medical Scientists
Projected employment change, 2023–2033: 16,800 more jobs
Job openings projected each year on average, 2023–2033: 8,900
Number of jobs, 2023: 146,600
Job outlook, 2023–2033: 11% (Much faster than average)
Median pay, 2023: $100,890/year
About the position: Medical scientists conduct research aimed at improving overall human health. They often use clinical trials and other investigative methods to reach their findings.
3. Biological Technicians
Projected employment change, 2023–2033: 5,500 more jobs
Job openings projected each year on average, 2023–2033: 10,300
Number of jobs, 2023: 83,100
Job outlook, 2023–2033: 7% (Faster than average)
Median pay, 2023: $51,430/year
About the position: Biological technicians help biological and medical scientists conduct laboratory tests and experiments.
4. Biochemists and Biophysicists
Projected employment change, 2023–2033: 3,200 more jobs
Job openings projected each year on average, 2023–2033: 3,100
Number of jobs, 2023: 35,700
Job outlook, 2023–2033: 9% (Much faster than average)
Median pay, 2023: $107,460/year
About the position: Biochemists and biophysicists study the chemical and physical principles of living things and of biological processes, such as cell development, growth, heredity, and disease.
5. Chemical Technicians
Projected employment change, 2023–2033: 3,200 more jobs
Job openings projected each year on average, 2023–2033: 7,300
Number of jobs, 2023: 58,300
Job outlook, 2023–2033: 5% (As fast as average)
Median pay, 2023: $56,750/year
About the position: Chemical technicians use laboratory instruments and techniques to help scientists analyze the properties of materials.
6. Epidemiologists
Projected employment change, 2023–2033: 2,100 more jobs
Job openings projected each year on average, 2023–2033: 800
Number of jobs, 2023: 11,000
Job outlook, 2023–2033: 19% (Much faster than average)
Median pay, 2023: $81,390/year
About the position: Epidemiologists are public health workers who investigate patterns and causes of disease and injury.
7. Microbiologists
Projected employment change, 2023–2033: 1,600 more jobs
Job openings projected each year on average, 2023–2033: 1,900
Number of jobs, 2023: 23,200
Job outlook, 2023–2033: 7% (Faster than average)
Median pay, 2023: $85,470/year
About the position: Microbiologists study microorganisms such as bacteria, viruses, algae, fungi, and some types of parasites.
8. Bioengineers and Biomedical Engineers
Projected employment change, 2023–2033: 1,500 more jobs
Job openings projected each year on average, 2023–2033: 1,400
Number of jobs, 2023: 19,700
Job outlook, 2023–2033: 7% (Faster than average)
Median pay, 2023: $10,730/year
About the position: Bioengineers and biomedical engineers combine engineering principles with sciences to design and create equipment, devices, computer systems, and software.
9. Zoologists and Wildlife Biologists
Projected employment change, 2023–2033: 800 more jobs
Job openings projected each year on average, 2023–2033: 1,500
Number of jobs, 2023: 18,800
Job outlook, 2023–2033: 4% (As fast as average)
Median pay, 2023: $70,600/year
About the position: Zoologists and wildlife biologists study animals—those both in captivity and in the wild—and how they interact with their ecosystems.
10. Genetic Counselors
Projected employment change, 2023–2033: 600 more jobs
Job openings projected each year on average, 2023–2033: 300
Number of jobs, 2023: 3,500
Job outlook, 2023–2033: 16% (Much faster than average)
Median pay, 2023: $95,770/year