While drugs like Roche’s Herceptin have greatly improved the prospects for people diagnosed with HER2-positive breast cancer, more than half of patients develop brain metastases. And because most drugs can’t cross the blood-brain barrier, treating the cancer once it has spread is challenging.
Researchers at Northwestern University combined chemotherapy with an investigational bromodomain (BET) inhibitor to target breast cancer that had spread to the brain in mouse models. The two drugs combined with radiation cleared the brain metastases in 75% of the animals, they reported in the journal Science Translational Medicine.
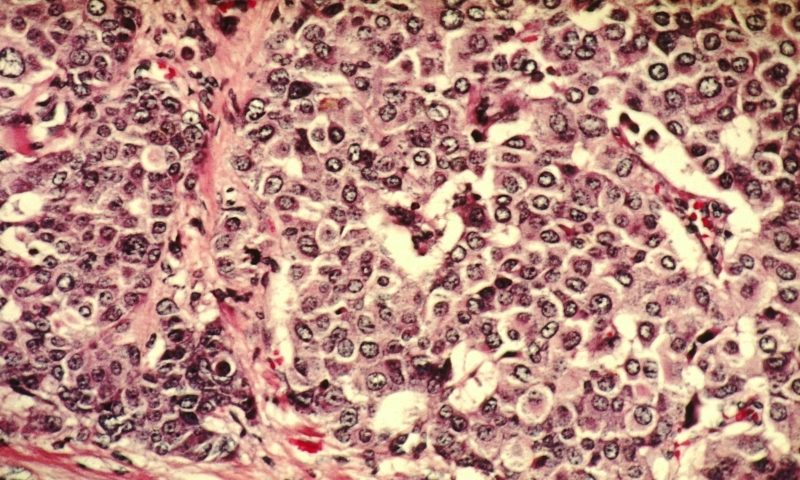
The combination the Northwestern team tried consisted of the chemotherapy drug vinorelbine and a BET inhibitor called I-BET-762. The BET inhibitor worked by increasing levels of beta-3 tubulin (TUBB3), a protein that’s found in brain metastases. That overexpression of TUBB3 improved the ability of the chemotherapy to target and kill the cancer cells in the brain, the researchers reported.
The Northwestern scientists discovered that BET inhibition lowered the expression of a transcription factor called myeloid zinc finger-1 (MZF-1) in brain metastases. That boosted levels of TUBB3, which in turn made the metastatic cells more likely to die in the presence of vinorelbine.
Other novel drug combinations are gaining steam in metastatic HER2-positive breast cancer. Seattle Genetics turned heads late last year with is data on Tukysa, which when added to Herceptin and capecitabine reduced the risk of disease progression or death in patients with brain metastases by 52%. The FDA approved the drug in April.
Several academic groups are investigating other methods for tamping down breast cancer metastasis. A team at Johns Hopkins University, for example, reported in July that combining antibodies that target the proteins KLRG1 and TIGIT with drugs that block DNA methyltransferases can reduce the spread of breast cancer by altering the behavior of natural killer cells.
The Northwestern team believes their preclinical work on the I-BET-762 combination with chemo and radiation should lead to a trial in people with metastatic HER2-positive breast cancer.
Patients with breast cancer that has spread to the brain are typically excluded from clinical trials because of their poor prognosis, but a trial of this combination could give those people “the chance to benefit from a new therapeutic regimen that has been proven to be strongly effective in experimental settings,” said lead author Maciej Lesniak, M.D., professor and chair of neurological surgery at Northwestern Medicine, in a statement.