Perimenopause explained: What it is, plus products that may help with symptoms

When it comes to health trends, menopause is having a long-overdue moment — and for good reason. It’s something half the population will experience, yet it’s been historically under-discussed. In fact, one study found that only 31% of doctors received menopause training in medical school.
Because of that, many women aren’t familiar with the stage that comes before menopause: perimenopause.
Perimenopause is when hormone levels — especially estrogen and progesterone — begin to fluctuate in the years leading up to menopause. And with that shift can come a host of confusing, sometimes disruptive symptoms, from hot flashes and night sweats to skin changes and mood swings.
Below, doctors explain what perimenopause is, how to tell if you’re in it, and what you can do to ease the transition. Plus, we share expert-recommended products that may help with common symptoms.
What is perimenopause?
Perimenopause refers to the transitional phase before menopause, according to the National Library of Medicine. It’s marked by shifting reproductive hormone levels — especially estrogen and progesterone — and typically starts in a woman’s 30s to 50s.
There’s no single test that confirms perimenopause, since hormone levels naturally fluctuate throughout the month. Instead, doctors assess your age, symptoms, and family history to make a diagnosis.
Symptoms of perimenopause
Perimenopause looks different for everyone — some experience intense symptoms, while others have a more gradual transition. Research suggests it begins about 5 to 10 years before menopause. Common symptoms include:
- Hot flashes and night sweats: Caused by hormonal shifts affecting the hypothalamus, your body’s temperature regulator.
- Irregular periods, vaginal dryness, and low libido: Estrogen and progesterone imbalances can impact the menstrual cycle and sexual health.
- Skin and hair changes: Lower estrogen levels reduce collagen and moisture, leading to dryness, thinning skin, and increased hair shedding.
- Mood swings and brain fog: Hormonal fluctuations can mimic the emotional volatility of adolescence.
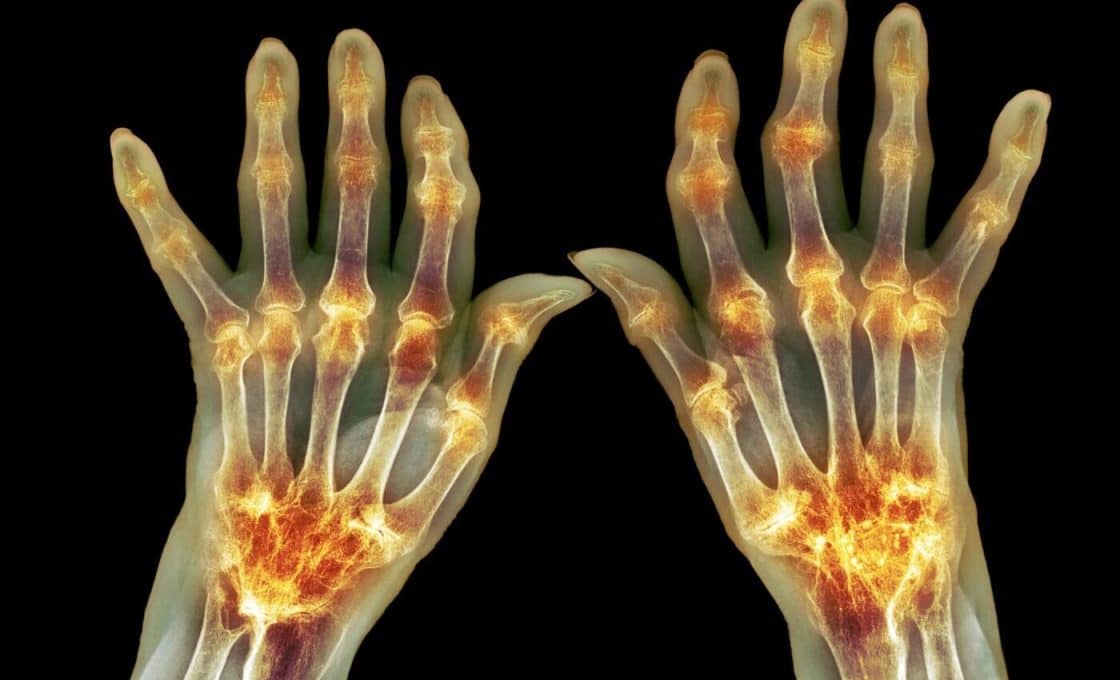
- Sleep issues, weight gain, joint pain, and frequent urination are also commonly reported.
What can you do about perimenopause symptoms?
You don’t have to tough it out — there are actionable ways to ease symptoms.
“The best thing you can do is approach aging with intention,” says Dr. Cristina Del Toro Badessa, a board-certified physician in integrative medicine. That includes eating well, exercising, limiting alcohol and caffeine, managing stress, and prioritizing sleep and relationships.
Some women benefit from supplements like collagen peptides or biotin, which may support skin and hair health. Others explore hormone replacement therapy (HRT), though it’s best discussed with a doctor.
There are also targeted products that can provide comfort and relief for specific symptoms — a few of our expert-approved picks are below.
Our top picks for perimenopause symptoms
While over-the-counter products are unlikely to eradicate symptoms, several things can make them feel more manageable. The following items were all created to address common perimenopause symptoms and are either highly recommended or recommended by an expert.
NBC Select reporter Zoe Malin is a fan of this personal cooling device and it can be a great tool to help you combat sudden hot flashes. The rechargeable fan is meant to be worn around your neck and, when turned on, it has vents that blow cool air toward you. It is also bladeless, so you don’t need to worry about hair getting caught. This fan has three airflow speeds, and you can change the angle of the vents to help the air blow where you want it.
Dealing with night sweats? These cooling sheets made our list of the best bed sheets. They are made with a cool-to-the-touch, moisture-wicking fabric to help regulate body temperature and mitigate sweat, according to the brand. Also lovely: They get softer the more you wash them, according to Sheex.
Experts previously told us it’s important to prioritize skin care products with hydrating ingredients when in perimenopause. This serum, which is made specifically for women in that stage of life, contains fatty acids to moisturize and vitamin C to brighten. It should be applied in the morning before using SPF and moisturizer.
If you’ve noticed perimenopause has led to dry, brittle hair, switching to a super hydrating conditioner can help. This one contains hydrating cupuaçu butter, which can also tame frizz and add shine, according to Biolage.
Ease joint aches with a massage gun. This one won an NBC Select Wellness Award last year and is a favorite amongst Select editors, including editorial director Lauren Swanson, who tested massage guns while marathon training. She said this one had heads and speeds that were gentle on tender muscles. It also has an ergonomic handle, making it easier to hold as you run it over your body and an LCD screen that makes the settings easy to read.