Helping Biomanufacturers Overcome Resistance to Modern Automation
Automation has a long history of driving enhanced production. During the Industrial Revolution, manufacturers first harnessed automated machines to increase yields for materials like cotton and paper. Decades later, the rapid expansion of the automobile industry in the early 20th century saw automotive companies streamline assembly lines, reducing assembly time from 12 hours to about 1.5 hours per car.
Today, robotic process automation plays a pivotal role in the life sciences industry. AI-powered technologies like machine learning have rejuvenated automation, enabling data-driven machines to control and interact with each other autonomously. Many industries are moving towards this goal. While these benefits are something for which they strive, greater quality and consistency are even more critical in the strictly regulated biopharma sector. So why has biopharma and the wider pharmaceutical industry been slower to adopt fully automated technologies?
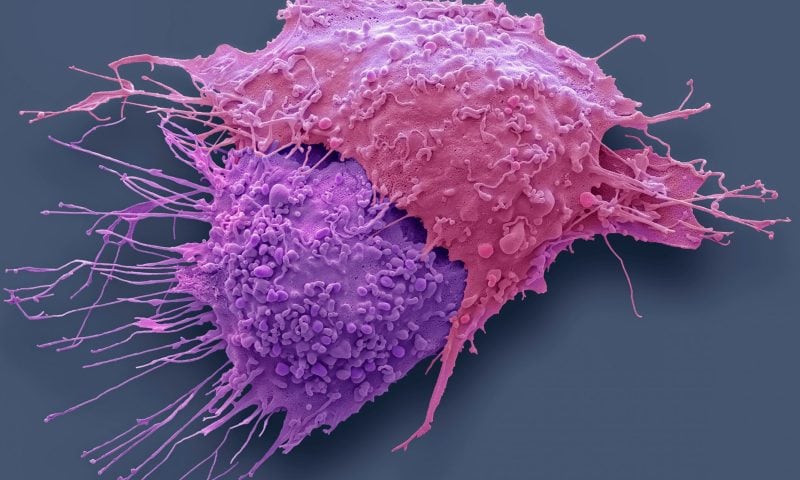
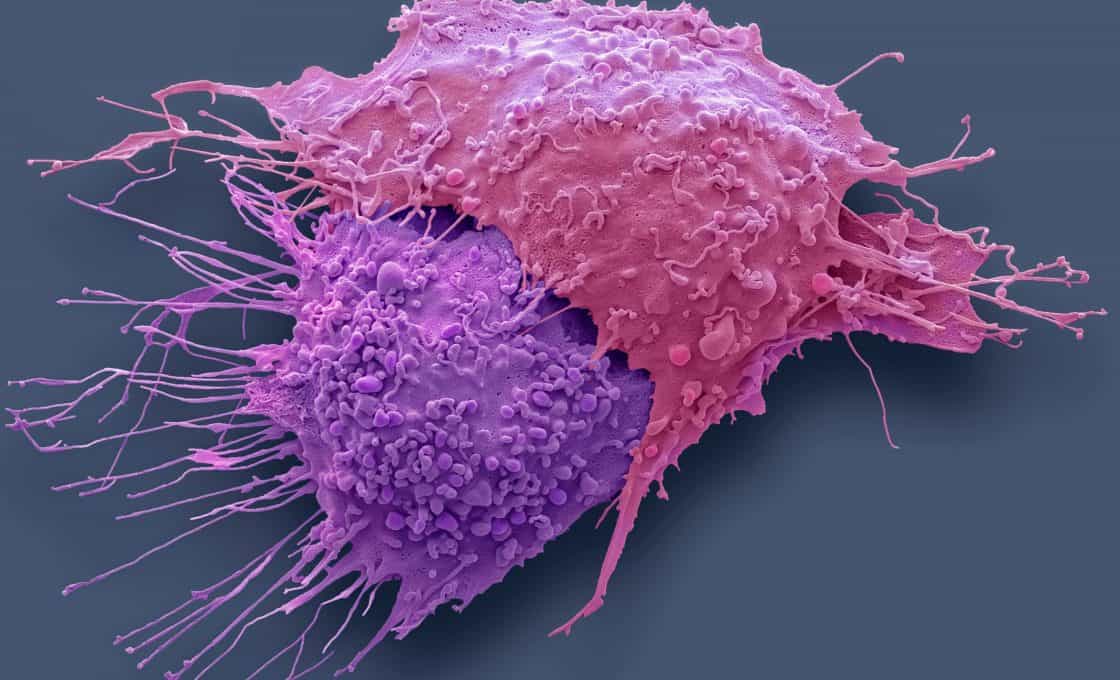
Complex and variable
The complexity and variability of bioprocessing are often cited as the main reason for the lag in uptake. However, success stories such as Moderna, which utilized automation and AI to develop an mRNA SARS-CoV-2 vaccine within a year, show it is achievable, without risking the quality and consistency that is so important to therapeutic manufacturing. Even with this compelling story, some firms opt for less-integrated options because they are simpler to deploy initially and align better to their current timelines, workforce, and budget.
The limited duration of patent protection is also a factor. Making major changes to a licensed facility can be challenging and time consuming. Once a facility is licensed to manufacture a biologics product, there likely won’t be multiple changes, and overhauling an entire factory can be cost prohibitive.
Additionally, there are different pressures on the biologics industry. For example, technology advancements are pivotal in reducing costs in the automotive industry. In the biopharmaceutical sector, the priority is on delivering products that maintain high quality, consistency, and reasonable pricing.
Because of the risk in changing a facility, automation is often considered in the design of new facilities. Modern biopharma facilities are constructed to be multipurpose, handling different products or production campaigns. Automation enables flexibility, allowing seamless transitions between different product lines without extensive manual reconfiguration. Automated systems can adapt quickly to different process parameters, making facilities more agile and future-proofing their operations.
Despite the advantages of automation, there are potential challenges to consider. Implementing fully automated systems can take time. Changeover times may present issues depending on how flexibly you’ve designed your systems and the facility to handle changes and multiple products. Legacy systems must be considered as many biopharma companies still rely on outdated, manual systems and integrating automation with these legacy systems can be expensive and technically challenging.
The data that automated systems generate needs to be integrated into existing data management and quality control systems. The transition from paper-based or manual tracking to automated digital systems can be slow and met with resistance.
Manufacturers may encounter difficulties when they adopt technology without clear objectives. However, aiming for continuous improvement of manufacturing processes is a clear and achievable objective. By consistently using technology to enhance processes and optimizing human and capital resources, manufacturers can achieve remarkable success.