Cancer, like the illicit drug trade, is hard to disrupt because it is a hierarchical operation. The low-level players are the easiest targets, but the high-level players would make the best targets—if only they could be reached. Too often, cancer’s high-level players work behind the scenes, pulling the strings of the low-level players, staying out of sight, and escaping any countermeasures.
Cancer’s high-level players may find that their luck is running out now that researchers at the University of Michigan Health Rogel Cancer Center have shown that it is possible to inhibit tumor growth by disrupting chromatin accessibility. Specifically, the researchers have found a way to degrade components of SWI/SNF, a chromatin remodeling complex. These components are ATPases that provide the energy SWI/SNF needs to unwrap DNA and expose enhancer elements that crank up the expression of cancer-driving genes.
In this scenario, the cancer-driving genes are the low-level players. They include androgen receptor (AR), FOXA1, ERG, and MYC. These genes essentially lose their high-level connection, SWI/SNF, when the ATPases are neutralized.
Details of the new anticancer approach recently appeared in Nature, in an article titled, “Targeting SWI/SNF ATPases in enhancer-addicted prostate cancer.” The paper makes the case that impeding SWI/SNF-mediated enhancer accessibility “represents a promising therapeutic approach for enhancer-addicted cancers.”
“[We] developed a proteolysis-targeting chimera (PROTAC) degrader of the SWI/SNF ATPase subunits, SMARCA2 and SMARCA4, called AU-15330,” the article’s authors wrote. “SWI/SNF ATPase degradation rapidly compacts cis-regulatory elements bound by transcription factors that drive prostate cancer cell proliferation, … which dislodges them from chromatin, disables their core enhancer circuitry, and abolishes the downstream oncogenic gene programs.”
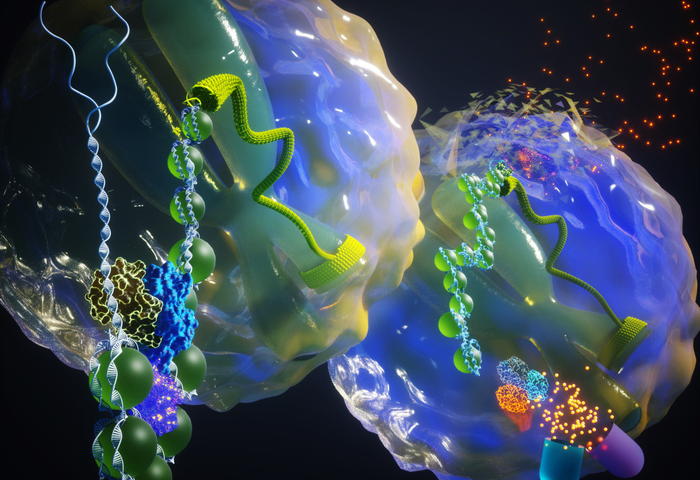
In human cells, DNA is tightly wrapped around histone proteins, collectively referred to as chromatin. These form a physical barrier to all DNA-based processes. Specialized protein machineries have evolved that consume energy and modulate the physical state of the DNA for its functional activation. These complexes work in close concert with DNA-binding regulatory factors called transcription factors to impart distinct cellular identity and function.
“This is the first demonstration in cancer that blocking access to chromatin can be pursued as an avenue to treat cancer,” asserted Arul M. Chinnaiyan, MD, PhD, the senior author of the Nature paper, the director of the Michigan Center for Translational Pathology, and the S.P. Hicks professor of pathology and urology at Michigan Medicine. “By compacting the chromatin around these enhancer elements, transcription factors are blocked from binding to the enhancer elements that drive cancer.”
The researchers looked at several prostate cancer models that expressed different oncogenes. They found that blocking the SWI/SNF complex slowed cancer cell growth and induced cell death especially in tumors driven by FOXA1 or androgen receptor. There was no effect on benign prostate cells.
“AU-15330 induces potent inhibition of tumor growth in xenograft models of prostate cancer and synergizes with the AR antagonist enzalutamide,” the researchers reported. “[It even induces] disease remission in castration-resistant prostate cancer models without toxicity.”
In normal development, the SWI/SNF complex is essential. “Normal cells can survive with default levels of gene transcription, but cancer cells are particularly addicted to these enhancer regions,” Chinnaiyan explained. “They need access to these enhancers to jack up the expression of oncogenic targets.”
Components of the SWI/SNF complex are mutated in a number of cancers, but rarely in prostate cancer. Prostate cancers driven by androgen receptor or FOXA1 were more sensitive to a SWI/SNF degrader than even cancers in which subunits were mutated.
“Without having mutations, and with just oncogenic transcription factors involved, prostate cancer cells were exquisitely sensitive to this degrader, even more so than lung cancer where a component of the pathway was mutated,” Chinnaiyan elaborated. “By disabling this SWI/SNF complex, we saw preferential activity against certain cancers and no toxicity in normal cells or normal tissues. This bodes well for clinical studies using compounds that target this pathway.”
It also suggests the possibility of using this approach for other types of cancer that are addicted to oncogenic transcription factors, including some multiple myelomas and other blood cancers.
The researchers used a SWI/SNF degrader in development by the Indian company Aurigene Discovery Technologies. These compounds are being developed for future clinical trials.
The Rogel Cancer Center team will continue to study the biology of this complex, help develop compounds that target this complex, and evaluate what other cancer types might respond to this approach. For prostate cancer, they are exploring in the laboratory a combination therapy using the SWI/SNF degrader with an anti-androgen therapy.