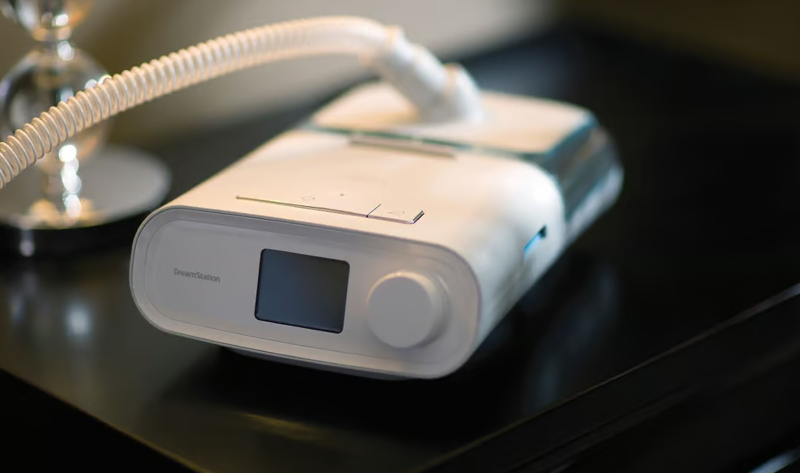
Nearly a year-and-a-half into Philips’ recall of about 5.5 million of its CPAP and BiPAP machines and other respiratory devices, complaints about the affected machines are still rolling in.
Between Aug. 1 and Oct. 31, the FDA received more than 21,000 new medical device reports (MDRs) from Philips, healthcare providers, consumers and patients, according to the agency’s latest update on the matter, published Tuesday.
Of those recall-related complaints, 91 included reports of patient deaths. Others described a range of non-fatal injuries, including cancer, pneumonia, asthma, infection, headache, difficulty breathing, dizziness, chest pain and more.
The recall began after Philips received dozens of reports describing how the polyester-based polyurethane foam used to muffle sound and vibrations in many of its respiratory devices could break down over time, sending potentially dangerous chemicals and debris into the airway—though documents submitted in court have since revealed that Philips knew about the foam breakdown issue at least a few years before beginning the formal recall.
In the decade prior to the recall’s mid-2021 start, Philips had passed on only 30 MDRs to the FDA between 2011 and April 2021, with no deaths or injuries among them. But in just the 19 months since then, the agency has racked up more than 90,000 complaints. More than half of the reports came in between May 1 and July 31 of this year, when the regulator tallied up around 48,000 MDRs sparked by the recall.
Including the 91 latest additions, the FDA has now received a total of 260 reports of death potentially linked to the faulty ventilators. About half, 126, were submitted between April 2021 and April 2022—a number that includes two more deaths than were originally tallied for the year, reflecting “Philips’ retrospective review of MDRs,” per the FDA. The remaining 43 patient death reports came in between May 1 and July 31, marking one fewer death than the period’s previously reported total.
Despite the overwhelming number of MDRs submitted in the wake of the Class I ventilator recall, the FDA has suggested they be taken with a grain of salt, since not all of the reported deaths and injuries may be specifically linked to the recall.
“The incidence, prevalence or cause of an event cannot typically be determined from this reporting system alone due to under-reporting of events, inaccuracies in reports, lack of verification that the device caused the reported event and lack of information about details such as frequency of device use,” the agency wrote.
With the latest influx of reports, the FDA said that it will be examining each of them in-depth, with a specific eye toward understanding why the reports continue to increase—and why the latest wave of patient death reports is more than double the size of the previous one.
One possible answer could be found in the rate of Philips’ efforts to notify all users of affected devices and begin repairing and replacing those devices—a rate that the FDA has repeatedly criticized for being too slow. Earlier this year, the agency issued an order forcing Philips to immediately alert all users and sellers of the affected machines about the recall, citing the company’s “inadequate” notification efforts.
In the months since, both the FDA and the U.S. Department of Justice have considered going even further. The former has suggested another order that would crack down on Philips’ ongoing repair-and-replace program, while the DOJ is currently in talks with the devicemaker about a proposed consent decree which, if taken to the extreme, could shut down production at certain manufacturing sites to resolve the recall-related issues.