As the coronavirus crisis lit up this spring, headlines about how the U.S. could innovate its way out of a pending ventilator shortage landed almost as hard and fast as the pandemic itself.
The New Yorker featured “The MacGyvers Taking on the Ventilator Shortage,” an effort initiated not by a doctor or engineer but a blockchain activist. The University of Minnesota created a cheap ventilator called the Coventor; the Massachusetts Institute of Technology had the MIT Emergency Ventilator; Rice University, the ApolloBVM. NASA created the VITAL, and a fitness monitor company got in the game with Fitbit Flow. The price tags varied from $150 for the Coventor to $10,000 for the Fitbit Flow—all significantly less than premium commercially available hospital ventilators, which can run to $50,000 apiece.
Around the same time, C. Nataraj, a Villanova College of Engineering professor, was hearing from front-line doctors at Philadelphia hospitals fearful of running out of ventilators for COVID-19 patients. Compelled to help, Nataraj put together a volunteer SWAT team of engineering and medical talent to invent the ideal emergency ventilator. The goal: build something that could operate with at least 80% of the function of a typical hospital ventilator, but at 20% or less of the cost.
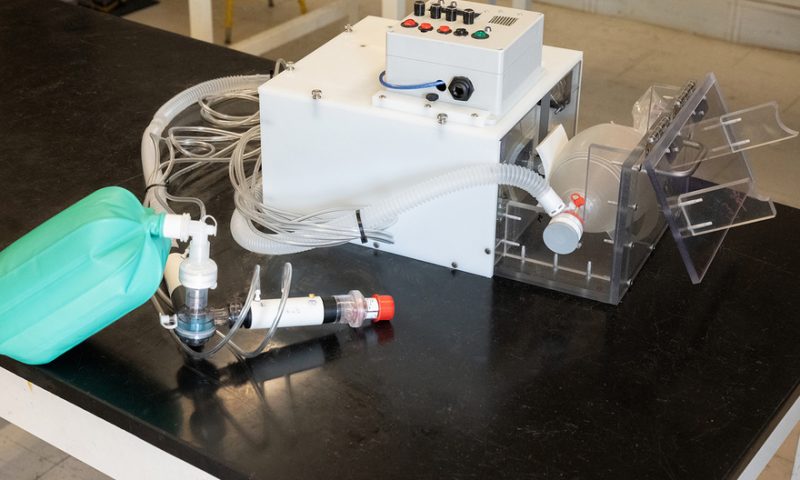
For decades, Nataraj has worked on medical projects—like finding a better way to diagnose a potentially deadly brain injury in premature infants—primarily with doctors at Children’s Hospital of Philadelphia and the Geisinger Health system in rural Pennsylvania, so key clinical players came together swiftly. By March 23, he had approached engineering faculty about collaborating on a monthslong effort to build the NovaVent, a basic, low-cost ventilator with parts that cost about $500. The schematics would be open-sourced, so others could use them free of charge to mass-manufacture the device.
The New Yorker wasn’t alone in referencing the ’80s TV series “MacGyver,” whose protagonist was a Swiss Army knife-carrying secret agent who got the job done with wits and whatever was at hand. The suggestion was that these ventilators were simple enough to throw together with parts from a medical supply closet or your neighborhood hardware store. “Everybody can make it,” one headline read, enticingly. These miracle machines, the thinking went, could be helpful in U.S. hospitals facing critical shortages, perhaps in cities surging with sick patients.
To understand the potential utility and true costs of these emergency ventilators, KHN followed Villanova’s team for three months as it developed, tested and prepared to submit the NovaVent for Food and Drug Administration approval.
The team tapped a maker of car parts along with roboticists. It gathered input from anesthesiologists as well as electrical, mechanical, fluid systems and computer engineers. It tapped nurses to help ensure that users would immediately know how to operate the ventilator. Local manufacturers 3D-printed pieces of the machine.
Nataraj and his team realized that some of the other ultra bare-bones machines wouldn’t meet the standards of the modern U.S. healthcare system. But they also believed there was a lot of room for Villanova’s team to innovate between those and the high-end, expensive devices from corporations like Philips or Medtronic.
One thing is clear: The $500 ventilator is something of a unicorn.
While the parts for the NovaVent cost about that much, the brainpower and people hours added uncounted value. In the early phases, the core group—all volunteers—worked 20 to 25 hours a week, Nataraj said, mainly via Zoom calls from home on top of their day jobs.
Teams of two or three were allowed into the lab to work—virtually the only people on campus. The effort, after all, was in line with the university’s Augustinian mission, which values the pursuit of knowledge, stewardship and community over the individual.
By the time they realized what they could achieve with the $500 model, the first wave of crisis had passed. Yet in those weeks, an alarm resounded across the land about the dismal state of America’s public health system.
So the NovaVent mission pivoted: build better low-cost vents for hospitals in poor and rural U.S. communities that have few, if any, ventilators.
One immediate legacy of the innovation happening at Villanova and elsewhere is the public-spirited nature of the effort, said Julian Goldman, M.D., an anesthesiologist at Massachusetts General Hospital who helps set standards for medical devices: “People from different walks of life in terms of their skills—engineers, clinicians, pure scientists—all thinking and working to try to figure out how to move very quickly to solve a national emergency with many dimensions: How do we make the patient safer? How do we make the caregiver safer? How do we deal with supply chain limitations?”
From other ventures, new designs have already been used as a jumping-off point to build emergency ventilators overseas. They’ve also bolstered New York City’s stockpile and could add to state and national reserves as well.
The early, urgent concerns about a looming ventilator shortage were well founded: On March 13, the U.S. had about 200,000 ventilators, according to the Society of Critical Care Medicine. But because of the surge of COVID patients, it was predicted the country could soon need as many as 960,000 (PDF).
In early April, New York Gov. Andrew Cuomo said the state would run out of ventilators in six days, leaving doctors with the sort of grim calculation they’d heard about from hard-hit northern Italy: “If a person comes in and needs a ventilator and you don’t have a ventilator, the person dies.”
In Philadelphia, 12 miles east of Villanova, hospital administrators braced for shortages and reported short supplies of the drugs required to sedate patients on ventilators.
President Donald Trump invoked the Defense Production Act to get major manufacturers to make ventilators, though GM was already working on it. When GM signed a $500 million contract to deliver 30,000 ventilators to the U.S. government by August, the NovaVent team wondered whether its own efforts would be futile.
“We said, ‘Well, GM is making it. Why are we making it?’” Nataraj said. “But there was a lot of uncertainty with the epidemiological models. We didn’t know how bad it was going to get. Or [the curve] could completely collapse and there’d be no need at all.”
And for a few weeks, it did seem the worst was over. The rate of new cases began to slow in the nation’s early epicenters. Hot spots flared in nearly every pocket of the country, but those too were mostly contained.
People spilled back into normal life, gathering in backyards, beaches and bars. In June, news coverage moved on to the calls for racial justice and mass protests after the videotaped killing of George Floyd in the custody of Minneapolis police.
In the background, the highly contagious coronavirus tore across the South, through Florida, Georgia, Texas and Arizona, and surged in California. Some states reported ICU beds were quickly at or above capacity. This mercurial virus had proved uncontrollable, and the prospect of ventilator shortages had bubbled up once again.
Past pandemics have been mothers of innovation. Progress in mechanical ventilation began in earnest after a 1952 polio outbreak in Copenhagen, Denmark. According to the American Journal of Respiratory and Critical Care Medicine, 50 patients a day arrived at the Blegdams Infectious Disease Hospital. Many had paralyzed respiratory muscles; nearly 90% died.
An anesthesiologist at the hospital realized patients were dying from respiratory failure rather than renal failure, as was previously believed, and recommended forcing oxygen into the lungs of patients. This worked—mortality dropped to 40%. But one big problem remained: Patients had to be “hand-bagged,” with more than 1,500 medical students squeezing resuscitator bags for 165,000 total hours.
“They’d recruit nurses and medical students to stand there and squeeze a bag,” says S. Mark Poler, M.D., a Geisinger Health system anesthesiologist on the NovaVent team. “Sometimes they were just so exhausted that they would fall asleep and stop ventilating. It was obviously a catastrophe, so that was the motivation for creating mechanical ventilators.”
The first ones were simple machines, much like the basic emergency-use ventilators created during the COVID crisis. But those came with hazards such as damaging the lungs by forcing in too much air. More sophisticated machines would deliver better control. These engineering marvels—the monitors, the different modes of ventilation, the slick touch-screen controls designed to minimize the risk of injury or error—improved patient treatment but also drove costs sky-high.
The emergency ventilators of 2020 focused on models that, typically, used an Ambu bag and some sort of mechanical “arm” to squeeze it. Most people are familiar with Ambu bags from scenes in TV programs like “ER” where paramedics compress the manual resuscitator bags to help patients breathe as they’re rushed inside from an ambulance. The bags are already widely available in hospitals, cost $30 to $40 and are FDA-approved.
But making machines that are that simple could render them effectively useless (or, worse, dangerous). Medical experts watching university and hospital teams coalesce across the country this spring to develop low-cost emergency ventilators took notice—and worried.
Goldman, the Massachusetts General anesthesiologist, was among the medical experts nervous about all the slapped-together ventilators.
“We had the maker community being stood up very quickly, but they don’t know what they don’t know,” said Goldman, chair of the COVID-19 working group for the Association for the Advancement of Medical Instrumentation, the primary source of standards for the medical device industry. “There were videos of harebrained ideas for building ventilators online by people who don’t know any better, and we were very concerned about that.”
The general public doesn’t really understand the nuances required to build a safe medical device, Goldman said.
“They look at something and think, well, this can’t be that hard to build. It just blows air,” he said. “‘I’ll take a vacuum cleaner and turn it on reverse. … It’s a ventilator!’”
AAMI wanted to encourage innovation, but also safety. So Goldman assembled a meeting of 38 engineers, regulators and clinicians to quickly write boiled-down guidelines for emergency-use ventilators.
The simplest ventilators were based on the idea of a piston in a car engine, Poler said: Put a piston on a crankshaft, hook it up to a motor and use a paddle or “arm” to compress the Ambu bag.
“It’s better than no ventilator at all, but it goes at one speed. It doesn’t really have any controls,” Poler said—not ideal when patients need to be monitored for changes in how their lungs are responding, or not, to treatment.
Villanova’s team of engineers, doctors and nurses realized that the simplest ventilators, the ones that AAMI was concerned about, seemed to ignore some basic, practical considerations: What sort of hospitals would these be used in, and under what conditions? What sorts of patients would be put on these ventilators? For how long? Would they be used as backups for higher-end ventilators? What about error alarms?
All good questions, Poler said, but the answer to all of them essentially is “we hope to never use these.”
Their best use? “A surge situation where you simply don’t have enough of the sophisticated ventilators.”
Rather than go totally bare-bones, the Villanova team designed the devices as though they would one day be deployed in modern healthcare.
Flow sensors, which monitor patient ventilation, cost several hundred dollars, so the team designed its own in the lab and 3D-printed it at a cost of 50 cents, Nataraj said, enabled by strides in 3D-printing technology that have vastly cut the price of so many devices. Southco, a Pennsylvania-based global manufacturer that makes parts like the latch on your car’s glove box, was tapped to use its 3D printers to make airflow tubes and couplings for the ventilator.
Garrett Clayton, director of Villanova’s Center for Nonlinear Dynamics and Control, was the day-to-day keeper of the prototype. He was particularly excited about the addition of a handle, which made it easier for him, and eventually others, to lug the 20-pound device from the lab to home and back.
Clayton’s computerized control system measures the flow rate of air going into the patient and converts it into volume, much as commercial ventilators do. That controls how hard and fast the Ambu bag is squeezed; it’s made of a hobby-grade Arduino microcontroller board. A direct-current motor attached to a linear actuator with a fist-shaped piece of PVC on the end pushes the bag in and out. The operator of the ventilator can control the respiratory rate (the number of breaths per minute), as well as the ratio between inspiration and expiration and the volume of air going in.
While traditional ventilators have many control methods, Clayton’s team focused on just one: how much volume is forced into the airway. “We have a set point so we don’t damage the lung,” he said.
Polly Tremoulet, a research psychologist and human factors consultant for ECRI and Children’s Hospital of Philadelphia, was pulled in to focus on error messages and make sure the ventilators’ buttons and displays “spoke the user’s language,” whether that user was an anesthesiologist in New Jersey or a nurse in India pulled into an ICU COVID ward.
Graduate student Emily Hylton and other nursing students were brought in to provide feedback about using the NovaVent and ask questions such as: Would all the controls and monitors look familiar to nurses at the bedside?
The very prospect of these low-cost devices is relatively new, Nataraj said, because of the price of microcontrollers with any real capacity: “Twenty years ago, they cost, oh gosh, $20,000—and now they’re $20.”
By May 30, the first NovaVent prototype was complete. It was successfully tested on an artificial lung at Children’s Hospital of Philadelphia on June 12. Villanova has applied for a patent for the NovaVent, to help ensure it won’t be commercialized by others.
“If you make it free without having a patent, other people can take it and charge for it,” Clayton said. “A patent protects the open-source nature of it.”
Once a provisional patent is received, the team will submit the ventilator for Emergency Use Authorization from the FDA—hewing to the guidelines set up by AAMI.
Within weeks of kicking off the NovaVent project, the curve in the East Coast had indeed flattened, and states had enough standard ventilators to treat every patient. The life-threatening ventilator shortage had not materialized. Some of the emergency-use ventilators based on designs by other teams, like the one at MIT, did go into production—but even those didn’t end up in hospitals, and instead went into city stockpiles meant to reduce potential future reliance on the federal government. So the Villanova team seized on a new, global mission.
“We thought if it wasn’t useful in the U.S. market,” Nataraj said, “we know the developing world, especially sub-Saharan Africa, Latin America and Central America, they don’t have the same kind of facilities that we do here.”
Where the ventilators might end up remains to be seen. Early on, Pennsylvania showed interest in helping Villanova find manufacturing partners. The team has spoken with engineers in India, Cambodia and Sudan (which reportedly has only 80 ventilators in the entire country) who are interested in possibly finding a way to manufacture the NovaVent.
Six thousand emergency ventilators based on the design by the University of Minnesota have been manufactured in the U.S., according to Stephen Richardson, M.D., a cardiac anesthesiologist who worked on that project. Three thousand were made by North Dakota aviation and agricultural manufacturer Appareo for state emergency stockpiles in North Dakota and South Dakota. UnitedHealth Group provided $3 million in funding to manufacture another 3,000 units made by Boston Scientific, which were donated to countries like Peru and Honduras through U.S. organizations; others were sent to the U.S. government.
Like the Villanova team, Richardson said he thinks the most promising potential for these ventilators is in developing countries.
“When we were arranging to get these donated to Honduras, we were speaking with a physician who was telling me that [at] his hospital right now, the med students are just hand-ventilating patients. For everything, and for COVID specifically,” Richardson said. “Right now, in Pakistan or in any low-resource country, a family member is hand-ventilating a toddler. Before COVID and after COVID, this is a problem.”
For Poler, the project was a reminder that the country needs to tend to its stockpiles. “People were thinking about [ventilator reserves] in the ’90s, and then they basically quit thinking about it,” he said. “COVID is a shocking reminder that we shouldn’t have stopped thinking about it.”
Goldman said the national efforts may not result in a flood of cheap ventilators in U.S. hospitals. International use could also be tricky. In countries with few resources, even very low-cost ventilators may not be feasible because of lack of electricity or compressed oxygen, though there is “potentially a sweet spot of need and capability where these things could be deployed.”
On the upside, he said, the pandemic kicked off a nearly unprecedented global engineering effort to share information and solve the problem.
“If there’s going to be a magic bullet to come out of this, it’s going to be the capability of our communities and our infrastructure,” he said. “People stood up, put in the appropriate processes and spirit, worked hard, made it happen. We’ve added resilience to the healthcare sector. That’s the outcome here.”
As for the NovaVent, team members were relieved they didn’t have to rush it into manufacturing as COVID-19 was ripping through the Northeast this spring, thanks to aggressive efforts to flatten the curve. “We ended up without a ventilator shortage, which is excellent,” Clayton said. “But with the increase in cases now, it’s very possible some of them may get used.”
To build on the project, Villanova is raising money for a laboratory for affordable medical technologies called NovaMed. The lab formalizes the process of making inexpensive medical equipment that follows the 80-20 function-to-cost rule. The university says the lab is “motivated by the belief that income should not determine who has access to lifesaving care.”
The effort to prevent a ventilator shortage, Nataraj said, made him think more critically about the American healthcare system overall.
“How come we haven’t built the technology, the economic and social systems that are able to handle a situation like this—especially when something like this was predicted?” he said. “It’s absolute nonsense. Why should a single person die because we weren’t prepared?”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.