Checkpoint inhibitors like Merck’s anti-PD-1 blockbuster Keytruda work well in patients with many types of cancers, but the drugs often become ineffective when tumors spread to the liver. But why?
Researchers at the University of California, San Francisco, made a discovery that helps answer that question—and they hit upon a combination treatment that looks promising in mouse models of liver metastases.
The UCSF team discovered that when tumors form in the liver, the cancer cells use the liver’s blood-filtering abilities to suppress the immune response to cancer. Combining a PD-1 inhibitor with a drug that inhibits another immune checkpoint—CTLA-4—restored the effectiveness of PD-1 inhibition in mouse models. They reported their findings in the journal Science Immunology.
The senior author of the study was Jeffrey Bluestone, Ph.D., adjunct professor of microbiology and immunology at UCSF and one of the researchers who originally led studies on CTLA-4 in the 1990s. Among his specialties is studying regulatory T cells, or Tregs, one of the few cell types in the body that can regulate the immune system in a targeted manner.
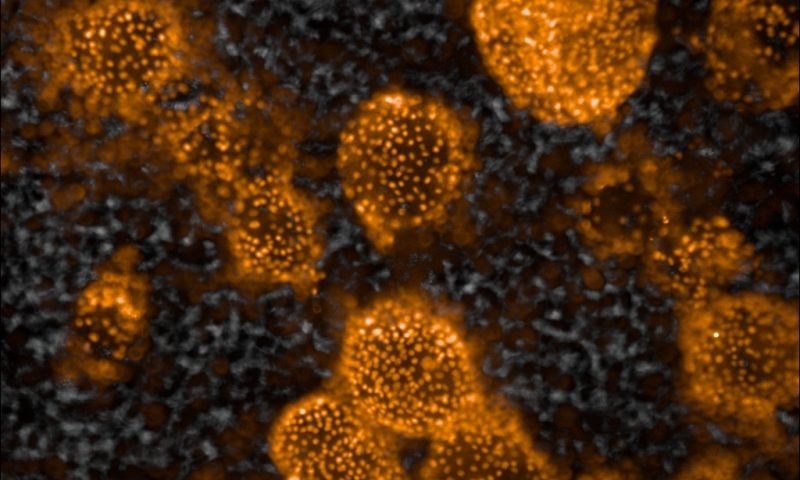
The UCSF team set out to determine the role of Tregs in liver tumors. First they implanted cancer cells under the skin of mice and in the lung or liver, so they could study the differences in response to anti-PD-1 treatments in each organ. Survival rates were lower in mice with liver tumors after PD-1 inhibition than they were in animals with lung tumors. Furthermore, in the mice with liver tumors, the skin tumors didn’t respond well to PD-1 inhibition either.
“It turned out that there wasn’t a difference in the quantity of Tregs between the skin tumors of mice with liver cancers and the mice without liver cancers. It was a difference in quality,” said lead author James Lee, M.D. a hematology and oncology clinical fellow at UCSF, in a statement.
Specifically, the liver tumors were able to change gene expression in Tregs, the UCSF team discovered. That altered several other immune cells, suppressing the ability of cancer-killing T cells to do their job.
From there, the researchers tested two drugs that block CTLA-4 in combination with a PD-1 blocker. Both CTLA-4 inhibitors restored the ability of the anti-PD-1 drug to unleash an immune response against liver tumors, but one was more effective than the other. The researchers suggested that the ability of that CTLA-4 blocker to act directly on Tregs and deplete them may have made the difference.
CTLA-4 inhibitors are already being combined with anti-PD-1 drugs in oncology practice. Bristol Myers Squibb’s PD-1 blocker Opdivo is approved along with its anti-CTLA-4 drug Yervoy to treat some patients with melanoma, lung cancer or colorectal cancer, for example.
The UCSF team hopes to try the I-O combination approach in patients with liver metastases who are unlikely to respond to traditional treatments.
Said Lee, “the liver can choose its enemy—what it wants to protect or not protect. What if, right from the start, you could use a drug that depletes Tregs as a complement to immunotherapy in patients with liver metastasis?”