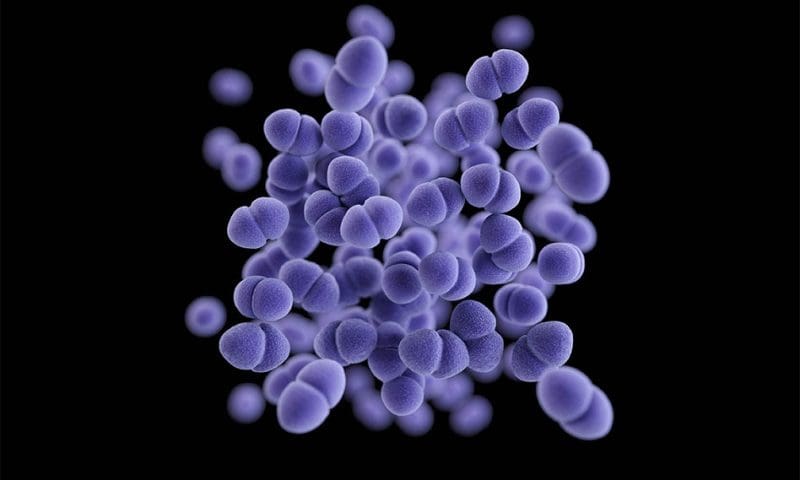
A drug-resistant strain of bacteria inhabiting hospital settings has evolved to utilize an antimicrobial genetic tool. Vancomycin-resistant Enterococcus faecium (VREfm) is responsible for many lethal infections and has been shown by researchers at the University of Pittsburgh (UPitt) to be equally lethal to other bacterial species.
The findings, published in Nature Microbiology in a study titled, “Bacteriocin production facilitates nosocomial emergence of vancomycin-resistant Enterococcus faecium,” suggest that VREfm have the ability to produce bacteriocin, an antimicrobial that can kill or inhibit other bacteria.
“Our lab has a front-row seat to the parade of pathogens that move through the hospital setting,” said senior author Daria Van Tyne, PhD, associate professor of medicine in UPitt’s Division of Infectious Diseases.
The Enhanced Detection System for Healthcare-Associated Transmission (EDS-HAT) was developed at UPitt and the University of Pittsburgh Medical Center (UPMC) to track infectious disease outbreaks using patient data. This machine learning system analyzes data from whole genome sequencing in conjunction with electronic health records to detect healthcare-associated outbreaks and investigate transmission routes.
“Once these strains are in an institutional setting—such as a hospital—and are matched up against other strains of VRE in a patient’s gut, they take over. It’s a ‘kill your buddies and eat their food’ scenario,” said first author Emma Mills, a graduate student in the Van Tyne lab.
VREfm is one of the deadliest hospital pathogens, killing approximately 40% of those infected. Given VREfm’s high mortality rate and resistance to treatment with common antibiotics, tracking its evolution is critical. The researchers leveraged EDS-HAT to study VREfm to help better understand its growth mechanism and elucidate strategies to reduce its spread and treat infected patients.
Over 700 samples of VREfm from UPMC were collected over a six-year period from 2017–2022 and analyzed with EDS-HAT to trace the evolution of VREfm within the hospital. The team found that while about eight VREfm strains were initially present in 2017, two specific strains began to dominate in 2018, and by the end of 2022, these strains accounted for 80% of VREfm infections. The key to their success was determined as the ability of these strains to produce bacteriocin T8, allowing these strains to outcompete others.
After expanding their analysis globally and analyzing a publicly available collection of 15,631 VREfm genomes collected between 2002 and 2022, the team found parallel results in the larger data set.
“This was a completely unexpected discovery—I was surprised to see such a dramatic signal,” said Mills.
The results confirmed that the bacteriocin-producing strains were not only overtaking the bacterial populations in UPMC but were also emerging as dominant strains globally.
Van Tyne commented: “When we took a step back and zoomed out, it quickly became apparent that big changes were afoot with one of the world’s more difficult-to-treat bacteria.”
While there is an increasing restriction of diversity of VREfm strains, it seems that clinically, the virility of the bacteriocin-producing strains has not increased. Patients are not more susceptible to increased illness or death from these strains. This could simplify the development of therapeutic measures.
“We may soon have only one single target for which to design therapeutics such as antibiotics or phage therapy,” pointed out Van Tyne. “It also suggests that bacteriocins are very potent, and perhaps we could weaponize them for our own purposes.”
The findings highlight the importance of tracking bacterial evolution and resistance mechanisms. By understanding VREfm’s evolution, researchers may be able to anticipate future threats and develop countermeasures before they become widespread.