A session at the American Association for Cancer Research (AACR) annual meeting posed a key question: Are cancer vaccines ready for prime time?
If you ask Scott Kopetz, M.D., Ph.D., of the University of Texas MD Anderson Cancer Center, the answer is a quick yes.
“I think they are. They’re ready,” Kopetz said in an interview with Fierce Biotech. His many titles include being deputy chair for translational research for the GI medical oncology department at the Houston hospital.
He clarified that vaccines are not ready to be standard of care but can be helpful in certain populations: “There’s a path forward. Years ago, I’m not sure I would have been comfortable to say that.”
Click here for more AACR 2024 coverage from the Fierce Biotech team.
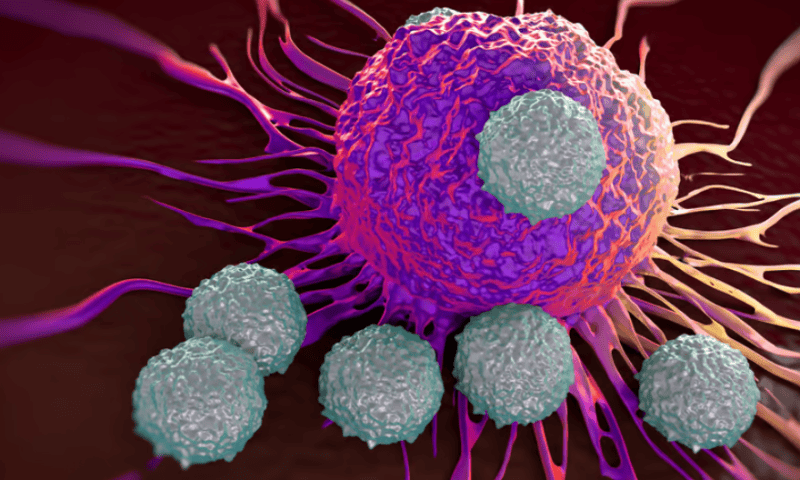
A quick clarification on what exactly a cancer vaccine is. This is not a shot in the arm that is going to prevent any random person from ever getting disease—although that would certainly be nice. Kopetz describes the cancer vaccines that are coming through the clinic now as an adjuvant treatment that can spur a T-cell response.
The primary goal is to tackle minimal residual disease, which is when cancer is not detectable on radiographical images, but malignant cells can be found via a blood test. This is particularly common in blood cancers but can also occur with solid tumors.
Cancer vaccines were the talk of oncology meetings like AACR years ago, but Kopetz said the technology just wasn’t ready. Companies ran into issues generating an effective T-cell response and then turning that into a benefit. Now, modalities like mRNA are helping spur more effective T-cell activation and allowing effective studies to be run, according to Kopetz.
Presenting at AACR’s Sunday press conference, hepatopancreatobiliary surgeon Vinod Balachandran, M.D., said the T-cell challenge is fourfold: to identify optimal antigens that are both tumor specific and immunogenic and to find a modular delivery platform that can address a rapidly evolving population of clones in patients that are fit enough and to sustain high magnitude tumor-specific T cells.
The T cells have to be able to recognize the cancer without recognizing the normal cells, said Balachandran, who practices at Memorial Sloan Kettering’s human oncology and pathogenesis program and is a member of the David M. Rubenstein Center for Pancreatic Cancer Research.
“This is a challenge, because host T cells are programmed to not respond to host tissues. Quite specifically, they are programmed to respond to the organism, such as pathogens. So a vaccine against an infectious pathogen is much more easy, if you will, because the T-cells are already preprogrammed to recognize them, expand and last,” said Balachandran.
Previous attempts were also unsuccessful, because companies didn’t quite have all pieces of the vaccine technology solved, according to Kopetz. That includes the delivery mechanism, payload and more. They were typically really good at one aspect of the technology but missing others.
“Right now, what we’re starting to see is the whole package,” Kopetz said.
Geneos CEO Niranjan Sardesai, Ph.D., who was at AACR to present his company’s data on a personalized cancer vaccine, said in an interview on the sidelines that the industry took notes during the early efforts and failures.
“What’s different is that we’ve learned from that at Geneos. We took the time to really understand the critical elements for what success will require,” he said
Geneos’ vaccine is DNA-based with a cytokine adjuvant IL-12 and an efficient delivery system to deliver the DNA plasmids into the cell, Sardesai explained.
Taking center stage
Much of the focus at AACR was on pancreatic cancer, where Kopetz said there’s a perfect matchup of an unmet need, minimum residual disease and a patient population that is prone to recurrence after surgery. This environment provides a good place to test out an adjuvant like a cancer vaccine.
That’s the space Balachandran is working in. He presented BioNTech’s much-buzzed-about research at the meeting, where the company provided the first glimmer of data on how long the vaccines might be able to last. In patients with resected pancreatic ductal adenocarcinoma—which has a five-year survival rate of about 8% to 10%—BioNTech’s autogene cevumeran was still providing a T-cell response at three years.
The company had previously presented efficacy data at the American Society of Clinical Oncology meeting last year showing that half of the treated patients posted a noticeable immune response, correlating with longer recurrence-free survival.
Speaking to that earlier paper, Balachandran said they are coming to understand why just 50% had an immune response. In fact, many of the patients who did not have a response did not have a spleen at the time of vaccination due to the standard of care in the indication. The next trial for the vaccine will include cohorts with and without a spleen to determine whether this is the cause.
BioNTech drew a crowd for its presentation, no doubt due to the fame garnered from the German company’s COVID-19 vaccine. Kopetz said the rise of mRNA is one of the reasons cancer vaccines have come back into the mainstream. The new technology has changed the game.
Moderna is also developing a vaccine called mRNA-4157 with Merck. The partners revealed plans for a phase 3 trial testing the vaccine in combination with Keytruda for post-surgery treatment of patients with resected melanoma that’s at high risk of recurrence in July 2023.
But these famed biotechs are not the only ones in the game.
Geneos presented data for a DNA personalized cancer vaccine for patients with unresectable, advanced metastatic hepatocellular carcinoma (HCC), where 10-year survival is only about 5%, according to Sardesai.
The trial featured 36 patients who received the vaccine and Merck & Co.’s Keytruda (also known as pembrolizumab), which spurred a 30.6% objective response rate. The response rate in this type of cancer is typically about 11% to 18%, Sardesai added. Three patients have had complete responses and one patient achieved secondary resectability, meaning a surgeon was able to go in again and remove the tumor.
“This has not been shown before,” Sardesai said. “What we’re showing is that cancer vaccine approach can drive meaningful clinical efficacy, even in patients who have advanced, unresectable disease.”
There are some caveats to the study: It’s an open label, single-arm trial. Geneos will need to do more robust testing down the line. But Sardesai is encouraged by the approximate doubling of responses than with Keytruda alone, which was determined via a historical control.
Geneos wanted to know more about why the vaccines are driving efficacy, so, in a paper published in Nature Medicine this week, the company examined the characteristics of the immune response. The analysis tracked the complete vaccination to clinical response cycle, showing a T-cell response that can be detected in the blood.
“These T-cells have the characteristics required for tumor killing,” Sardesai said. “This is such a bad prognosis for patients that to see meaningful tumor reductions by MRI radiological imaging has been pretty profound.”
The study has not yet matured to the point of providing durability data, but Sardesai said that about half of the patients are still being followed for overall survival and almost a third are still being treated.
“We set up the study with the idea of treating patients for two years because pembrolizumab per label is for two years and then these patients have a median survival of 13 to 15 months. But we’ve now extended the protocol to continue treating these patients beyond two years because these patients are doing so well,” Sardesai said. Patients dropped Keytruda at two years but have kept on with the vaccine.
Another key is safety in these populations. Geneos’ vaccine had a safety profile that suggests it can be added with little impact for patients, the CEO said.
Geneos’ next step is to set up a randomized controlled phase 2 trial in HCC that compares the personalized vaccine with a PD-1 inhibitor like Keytruda directly against a PD-1 inhibitor alone.
“People talk about the future of cancer vaccines or prospects of cancer vaccines. I firmly believe that the time for cancer vaccines is here and now,” Sardesai said. He’s also pleased to see his peers touting efficacy in earlier stages of disease.
There are still a lot of questions to be answered. While BioNTech helped fill in a piece of the puzzle with the durability data, Kopetz said more data and larger studies are needed. He would also like more emphasis on designing the registrational phase 3 trials to demonstrate a clear benefit, particularly early after administration. More consideration needs to be put into the best combination approaches, too.
Kopetz said cancer vaccines will likely always be used in conjunction with other therapies, but maybe someday they could be administered alone.
Of course, the bigger question still remains: Will we someday have a vaccine to truly prevent cancer? Kopetz hopes to see vaccines move into cancer hereditary populations, but that’s not quite ready for prime time at the moment.
While oncologists can follow confirmed disease with various biomarkers, with no disease, there’s no real biomarker to follow. Not to mention, such a trial would be very lengthy and resource intensive.
So it all comes back around to designing the perfect trial, Kopetz said.