Despite the availability of multiple FDA-approved immunotherapies that leverage the body’s immune system to fight cancer, only a fraction of cancer patients are benefiting. That’s because cancer cells are cunning. They develop strategies to avoid being targeted and destroyed by immune cells.
To understand the genetic drivers behind the ability of cancer cells to evade the immune system, scientists at the University of Toronto, in collaboration with Agios Pharmaceuticals, used CRISPR to screen six genetically diverse mouse cancer cell lines. They found that genes involved in autophagy—a process where cells recycle damaged components to regenerate themselves—were key for immune evasion.
The researchers suggested that their findings, published in Nature, open up new venues for the development of immunotherapies that could be effective for large patient populations across several different tumor types.
“It’s very important to understand at the molecular level how cancer develops resistance to immunotherapies in order to make them more broadly available,” said University of Toronto professor Jason Moffat, Ph.D., the study’s corresponding author, in a statement.
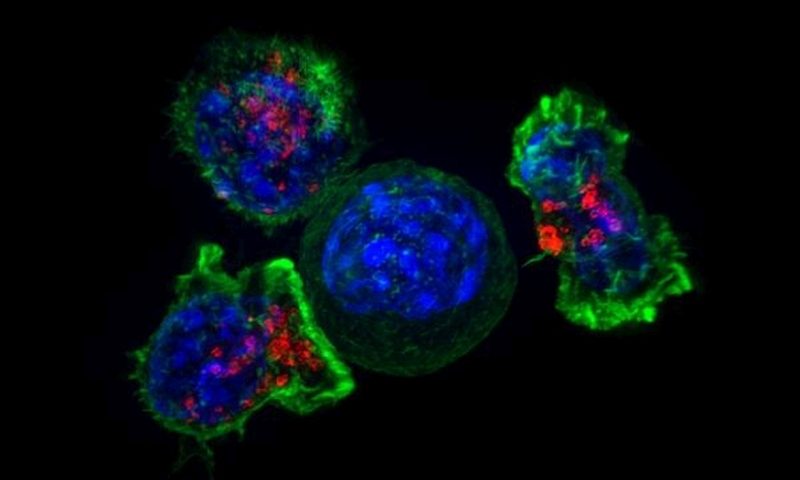
Moffat and colleagues used CRISPR to screen cancer cells that were cultured in the presence or absence of preactivated killer T cells—immune cells with a natural ability to hunt and kill cancer. They identified 182 genes that, when deleted, increased either the sensitivity or the resistance of cancer cells to T cells. They called them “core cancer-intrinsic cytotoxic T lymphocyte-evasion genes,” because every one of them was present across at least three of the six cells lines that the team screened.
The core set of genes included several genes that were known to affect signaling of interferon gamma, a cytokine that’s critical to an array of immune responses and that serves as a master communicator with several types of immune cells. Three negative regulators of the interferon-gamma response—Socs1, Ptpn2 and Adar—also emerged as immune-evasion genes.
Several genes identified were related to autophagy. Among the top hits was the Fitm2 gene, which is required for normal fat storage in adipose tissue in mice but was not previously associated with interferon-gamma signaling.
In two mouse models of renal cell carcinoma and melanoma, cancer cells with deleted Fitm2 showed increased cell death after treatment with interferon gamma compared with control cells, the team reported.
Surprisingly, the researchers also found that deleting certain autophagy genes in pairs could make the cells resist T-cell killing. For example, cells that lacked both Atg12 and Atg5 were strongly resistant to the killing effects of T cells as compared with single-mutant cells. This means that if a tumor already harbors a mutation in one autophagy gene, an immunotherapy that targets another autophagy gene could make the disease worse, the researchers explained.
Other oncology researchers are also focusing on the autophagy. A team from the University of Cincinnati, for example, found that mutations in mitochondrial complex I could prevent the autophagy that’s triggered by mTOR inhibitors. And researchers at the University of North Carolina reported that targeting the KRAS mutation in pancreatic cancer with an MEK inhibitor made cancer cells more dependent on autophagy for survival. They blocked the process with the anti-malaria drug hydroxychloroquine.
The University of Toronto-led team believes its list of 182 core immune-evasion genes may inform efforts to develop novel cancer immunotherapies. The scientists stressed the need to explore how combined genetic interactions may alter cancer’s immune-evasion activity. While simultaneous control of certain genetic features may sensitize cancer cells to immunotherapy, it could make the disease worse in others, they warned.