Tumor cells are better at forming potentially deadly metastases when they move as part of clumps rather than on their own. But the molecular mechanisms driving the aggressive growth of these multicellular tumor clusters are unclear.
Now, scientists at the Fred Hutchinson Cancer Research Center have identified a signaling chamber among clustered breast cancer cells. The chamber facilitates communication and cooperation among the clusters, which drives metastatic disease. They published the findings in a Cell paper.
Genetically suppressing a molecule involved in cluster signaling reduced the outgrowth of primary tumors and metastases in mice, the team reported. Armed with that knowledge, the researchers are now looking for drugs to block that signal in the hopes of stopping metastasis in breast cancer.
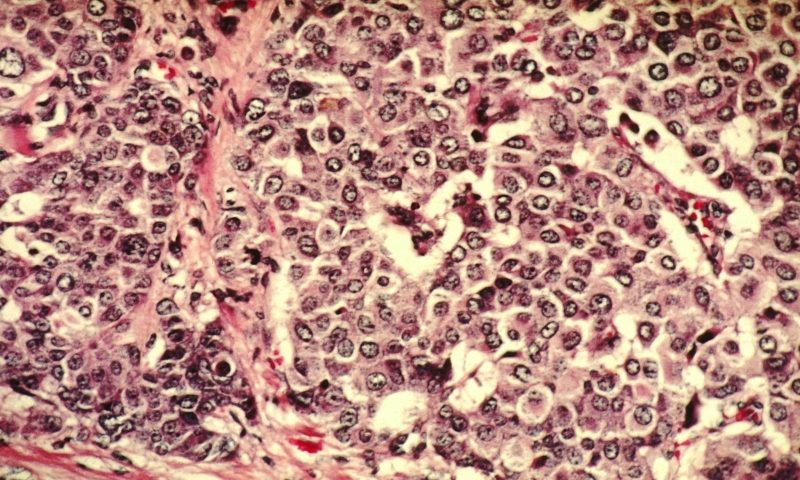
In a mouse model of breast cancer, the Fred Hutch researchers found that tumor clusters grown in lab dishes formed 532-fold more lung metastases than did an equal number of single cells. These clusters also appeared to have a much higher rate of survival than did single cells. So, they set out to understand the mechanisms behind the aggressiveness of the clusters.
RNA sequencing of the breast cancer cells throughout their aggregation from single cells to highly metastatic clusters revealed that the EPGN gene coding for the protein epigen was the most upregulated gene. Epigen is a signal that acts on the notorious cancer growth receptor EGFR.
Using electron microscopy, the researchers found that epigen accumulated in tiny spaces between the cells. They named these cavities “nanolumina.” Within nanolumina, epigen acted as a liaison between neighboring cancer cells, helping transmit growth signals.
“It’s sort of a nanoscale microenvironment, a localized signaling environment between cells,” Kevin Cheung, the study’s senior author, explained in a statement.
Epigen acts like a switch for proliferation and migration of tumor cell clusters, the team showed. When epigen was present, the clusters divided and grew. But when their EPGN gene was removed, the clusters showed markedly increased migration but reduced growth.
In mice with aggressive breast cancer cell clusters, tumors without EPGN grew significantly slower and there were fewer lung metastases than what was observed in the control animals, even though there was an initial seeding of distant metastases, the team reported.
Other research groups have examined different methods for stopping breast cancer metastasis. A team at Northwestern University recently showed that an investigational BET inhibitor called I-BET-762, by lowering the expression of a transcription factor called MZF1, made brain metastases in breast cancer more vulnerable to the chemotherapy drug vinorelbine.
As for preventing breast cancer cells from forming metastases, a Johns Hopkins team found that combining inhibitors of DNA methyltransferases with antibodies targeting TIGIT or KLRG1 could prevent metastasis by altering a process by which breast cancer cells evade natural killer cells. Another team at Fred Hutch suggested that inhibiting proteins called integrins could help kill off dormant breast cancer cells before they wake up and cause metastases.
Cheung and colleagues have observed increased epigen expression and nanolumina formation in triple-negative breast cancer. The team now hopes to identify drugs that can target nanolumina and stop the over-expression of epigen in a bid to potentially slow the growth of tumor clusters.
From there, the researchers plan to investigate whether the nanolumina phenomenon is a factor in other aggressive cancer types.