Immunotherapy has been one of the most promising advancements in cancer treatment. However, consistency in immunotherapy treatment effectiveness remains a formidable challenge. Now, Cancer Center at Illinois member Kun Wang, Binbin Wang, a post-doctoral researcher at the National Cancer Institute, and Robert Saddawi-Konefka, a physician-scientist at MD Anderson Cancer Center (formerly at UCSD) are taking the guesswork out of cancer treatments through a predictive model for determining immunotherapy treatment effectiveness.
The researchers have introduced a blood-based liquid biopsy model, called the Liquid Biomarker of Immunotherapy Outcomes (LiBIO) score, which allows researchers to predict how likely patients are to respond to immune checkpoint blockade (ICB) drugs, an immunotherapy treatment.
The work is published in the journal Nature Communications.
“Immunotherapy is a promising cancer treatment strategy that tunes the immune system to recognize and attack cancer cells,” said Kun Wang, assistant professor of comparative biosciences and bioengineering (affiliated). “It has become an important treatment option for patients with head and neck cancer; however, not all patients benefit, and researchers still lack a reliable, non-invasive biomarker to predict response.”
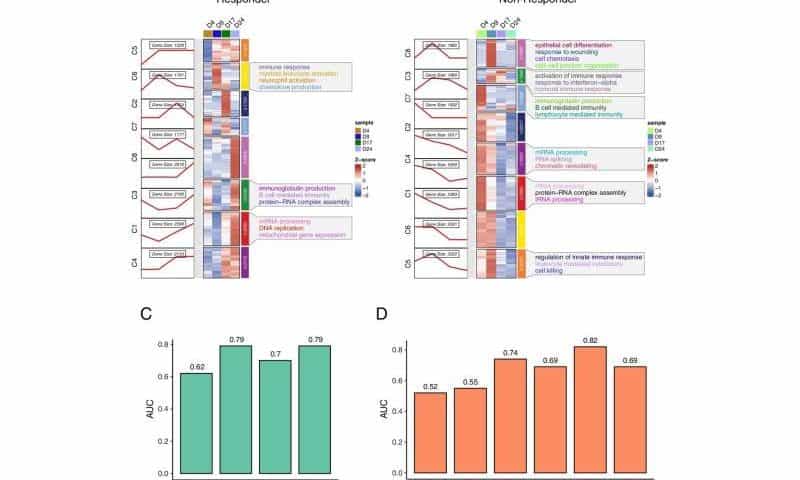
Researchers used a mouse model of head and neck squamous cell carcinoma (HNSCC) and utilized liquid biopsies to continuously track changes in the mice’s immune system before and after the implementation of ICB treatment. It was found that an early increase in specific cancer-fighting immune cells (effector memory T cells and B cells) was strongly correlated with a positive response to ICB treatment.
“We identified an early post-treatment time point as optimal for assessing treatment response,” Wang said. “This led to the identification of a gene signature set reflecting effector memory T and B cell populations linked to immunotherapy response at this critical time point, serving as a potential liquid biomarker.”
The LiBIO score has a much higher success rate in determining treatment effectiveness compared to previous biomarkers and has been successful in many other forms of cancer including breast cancer, lung cancer, and melanoma.
“This biomarker can help identify patients who are more likely to benefit from immunotherapy, thereby improving treatment efficacy and reducing the burden of unnecessary treatment,” Wang said. “Because it is blood-based, it also offers a non-invasive way to monitor treatment progress at the molecular level, which is especially valuable for real-time clinical decision-making.”
With the promising outcome of this mouse model, the next step is bringing the use of LiBIO scores to human patients in clinical trials. Researchers are hopeful that human trials are not too far in the future, though there is no definitive timeline.
“My collaborator and friend, Dr. Robert Saddawi-Konefka, who is also a co-first author of the paper, is an exceptional physician–scientist at MD Anderson Cancer Center,” said Wang. “He is currently working on a proposal and collaborating with other physicians to initiate human trials based on this research.”
Despite uncertainties and current limitations in this line of research, scientists remain optimistic about what the use of the LiBIO score means for the future of immunotherapy in the treatment of several types of cancers.
“While we found that the combination of effector memory T cells and B cells, and even their TCR and BCR repertoires, can be predictive of immunotherapy response, the underlying reason why B cells enhance T cell-mediated responses remains unclear,” said Wang.
“We aim to investigate the interactions between B cells and T cells to uncover the mechanism behind this synergy. Understanding this could enable the development of combination immunotherapies designed to strengthen their interaction and improve treatment outcomes.”