After meals, the intestines use peristalsis to move food through the gut using coordinated contractions and relaxations of smooth muscle. Results from a new study in mice done by scientists at Harvard Medical School (HMS), the Icahn School of Medicine at Mount Sinai, and their collaborators show that a pressure-sensing protein called Piezo1 in intestinal nerve cells plays a key role in coordinating these movements and preventing inflammation in the gut. Details are published in a new Cell paper titled, “Enteric neuronal Piezo1 maintains mechanical and immunological homeostasis by sensing force.”
If the findings can be replicated in humans, scientists believe that they could inform the design of new treatments for intestinal inflammation in IBD patients as well as for disorders of gut motility such as diarrhea and constipation. Ruaidhrí Jackson, PhD, an assistant professor of immunology at HMS and co-senior author on the study, noted that the findings show how the nervous and immune systems interact in the gut to maintain healthy function and protect against inflammation. The results also add to a growing body of research showing that these two systems engage in a powerful interplay in various organs, including the brain, lungs, and skin.
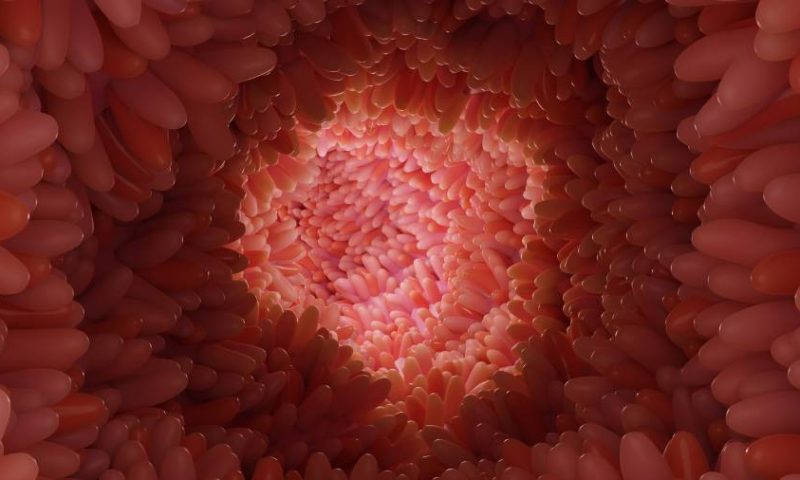
The question is how the intestines can move independently without input from the central nervous system. Previous studies have shown that enteric neurons—nerve cells contained completely within the intestines—interact with smooth muscle cells to drive peristalsis, but exactly what happens at the interface has been unclear.
Jackson had previously studied the role of the Piezo1 protein in immune cells that sense the mechanical force generated by breathing. He and other colleagues published a study in Nature in 2019 that highlighted how the protein can spur inflammation in the lungs when it senses mechanical pressure. He wondered if this protein could also be somehow involved in digestive peristalsis.
To explore this idea, researchers in the current study analyzed gene activity in mouse and human gut neurons. They found evidence that the gene that produces Piezo1 is highly active in excitatory gut neurons, which are responsible for triggering muscle contractions in the intestine by releasing the chemical messenger acetylcholine.
To better understand the role of the protein, the researchers tested mouse intestinal tissue under varying pressure conditions. In normal mice, the intestines contracted when pressure increased. In mice that were genetically altered to lack the gene for the protein, scientists observed that the tissue failed to contract under pressure. This confirmed that Piezo1 acts as a pressure sensor, helping regulate gut movement.
For their next set of experiments, the researchers used genetically modified mice whose gut neurons could be altered by light. When Piezo1-expressing neurons were activated by light, the mice expelled a small glass bead from their intestines twice as fast as normal mice. When the researchers used chemicals to turn off Piezo1 neurons in the gut, digestion in these mice slowed notably.
Once they confirmed the role of Piezo1 in gut movement, the researchers then assessed the impact of exercise and gut inflammation due to intestinal bowel disease (IBD) on the protein’s activity. Running on a treadmill increased the movement of waste through the intestines in mice with functional Piezo1 protein. These mice had bowel movements after just 10 minutes of exercise. Mice who lacked the protein did not have a similar increase in intestinal motility. It suggests that the gene for Piezo1 senses the increased intestinal pressure from exercise.
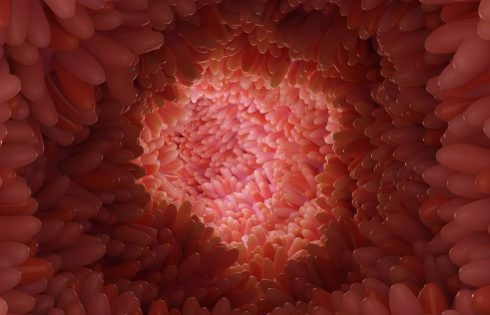
To test Piezo1’s role in IBD, the researchers created mouse models of the disease. Mice with IBD whose guts had intact Piezo1 produced a bowel movement more quickly, compared with animals in which Piezo1 was inactivated. In addition, turning off the gene also worsened IBD symptoms. Compared with mice that had intact Piezo1 genes, animals without working Piezo1 lost more weight and gradually lost the layer of protective intestinal mucus and mucus-making cells that shield the walls of the colon.
The scientists hypothesize that the worsened inflammation could be due to the loss of acetylcholine, which is responsible for nerve signaling and smooth muscle movement and also acts as an anti-inflammatory agent. Jackson suspects that IBD-linked inflammation might spur Piezo1 to cause enteric neurons to generate excess acetylcholine in an effort to tamp down inflammation, and this results in the increased intestinal motility characteristic of this condition.
Modulating Piezo1 activity might be a way to fight IBD inflammation, Jackson said. A possible treatment could target Piezo1 in gut neurons to release acetylcholine. This strategy would be markedly different from the way most IBD drugs work, which is by suppressing key inflammatory proteins. He and his colleagues plan to explore these kinds of therapies in future studies.