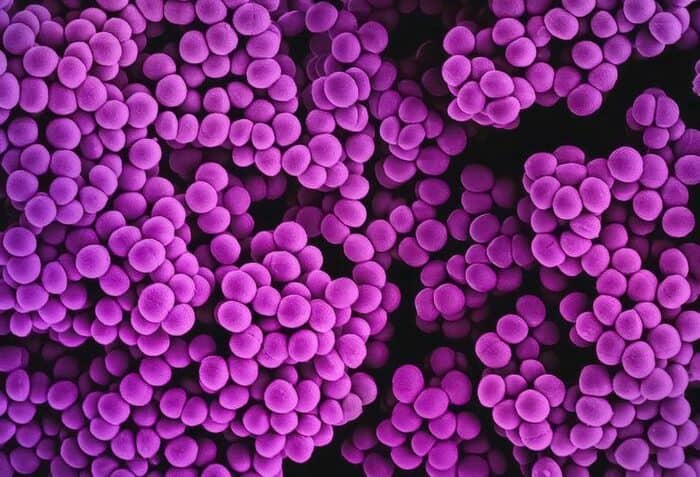
Staphylococcus aureus is a leading cause of antibiotic resistance-associated infections and deaths. It is also the most prevalent bacterial infection among individuals with diabetes mellitus (DM), a chronic condition that affects blood sugar control and reduces the body’s ability to fight infections.
A study by scientists at the University of North Carolina School of Medicine found that in diabetic mice with an S. aureus skin and soft tissue infection (SSTI), the bacterium evolves antibiotic resistance rapidly, whereas resistance didn’t occur in nondiabetic mice over the course of infection. Results from the study, headed by microbiologists Brian Conlon, PhD, and Lance Thurlow, PhD, showed how the diabetic microbial environment produces resistant mutations. The findings also demonstrated that controlling the blood sugar of diabetic mice with insulin resulted in significantly decreased incidence of antibiotic-resistant S. aureus. The study results point to potential approaches to combatting antibiotic resistance in individuals with diabetes.
“We found that antibiotic resistance emerges much more rapidly in diabetic models than in nondiabetic models of disease,” said Conlon, associate professor at the department of microbiology and immunology. “This interplay between bacteria and diabetes could be a major driver of the rapid evolution and spread of antibiotic resistance that we are seeing.”
Conlon, Thurlow, and colleagues reported on their study in Science Advances. In their paper, titled “Diabetes potentiates the emergence and expansion of antibiotic resistance,” the team noted, “In total, this work establishes a direct relationship between diabetes and the emergence and proliferation of AMR … The data presented here may inform the development of treatment strategies and highlight the crucial need for the development and implementation of more effective antibacterial compounds to improve infection outcomes in individuals with diabetes.”
Antibiotics are powerful, fast-acting medications designed to eradicate bacterial infections. However, in recent years, their dependability has waned as bacterial resistance spreads. People with DM are more susceptible to bacterial infection, leading to a high frequency of severe and chronic infections in individuals with DM, the authors noted. “Individuals with diabetes mellitus frequently develop severe skin and soft tissue infections (SSTIs) that are recalcitrant to antibiotic treatment … Antimicrobial resistance (AMR) further complicates the treatment of infection in individuals with DM.”
Diabetes affects the body’s ability to control glucose, often causing excess glucose to build up in the bloodstream. Staph feeds off these high sugar levels, allowing it to reproduce more rapidly. “S. aureus uses glucose as a preferential carbon source and becomes hypervirulent in a diabetic SSTI infection,” the scientists further stated. The bacterium can also grow without consequence, as diabetes also impairs the immune system’s ability to destroy cells and control infection. “The increased susceptibility to infection in individuals with diabetes is due to a combination of factors including immunosuppression, hyperglycemia, and lack of vascularization in the extremities,” the scientists further explained. SSTIs in diabetic individuals are frequently severe and may necessitate amputation, especially in the extremities such as toes and feet.
As the numbers of bacteria increase in a diabetic infection, so does the likelihood of resistance. Random mutations appear and some build up resistance to external stressors, like antibiotics. Once a resistant mutant is present in a diabetic infection, it rapidly takes over the population, using the excess glucose to drive its rapid growth.
“Staphylococcus aureus is uniquely suited to take advantage of this diabetic environment,” said Thurlow, assistant professor of microbiology and immunology, with joint appointments in the UNC School of Medicine and the Adams School of Dentistry. “Once that resistant mutation happens, you have excess glucose and you don’t have the immune system to clear the mutant and it takes over the entire bacterial population in a matter of days.”
Conlon, an expert on antibiotic treatment failure, and Thurlow, an expert on Staph pathogenesis in diabetes, have long been interested in comparing the effectiveness of antibiotics in a model with and without diabetes. Using their connections within the department of microbiology and immunology, the researchers brought their labs together to perform a study with antibiotics in a diabetic mouse model of S. aureus infection.
First, the team prepared a mouse model with bacterial SSTIs. The mice were divided into two groups: one group was given a compound, streptozotocin (STZ), that selectively kills cells in the pancreas, rendering the animals diabetic, and the other group was not given the compound. Researchers then infected both diabetic and non-diabetic mice with S. aureus and treated the animals with rifampicin, an antibiotic to which resistance evolves at a high rate.
After five days of infection, the authors noticed that the rifampicin treatment had practically no effect in diabetic models. Testing samples the team found that the bacteria had evolved to become resistant to rifampicin, with the infection harboring over a hundred million rifampicin-resistant (RifR) bacteria. The mutation had taken over the entire infection in just four days. In contrast, there were no rifampicin-resistant bacteria in the nondiabetic models. “… we did not detect the emergence of any RifR S. aureus in non-diabetic mice,” the team further noted.
They next inoculated diabetic and non-diabetic models with S. aureus as before, but this time supplemented with a known number of rifampicin-resistant bacteria. While these bacteria rapidly took over the diabetic infection, they remained as only a sub-population in non-diabetic models after four days of rifampicin treatment. “… our data suggest that only in a diabetic environment under antibiotic pressure can this RifR mutant thrive and expand,” the investigators stated.
While the findings have left the team with questions, they maintain that the evolution of antibiotic resistance in people with diabetes could spell trouble for the population at large. Antibiotic-resistant strains of bacteria spread from person to person in the same ways as other bacteria and viruses do—in the air, on doorknobs, and the food that we eat—which makes preventing these types of infections a major priority. “The rapid growth of the diabetic population combined with the concurrent rise of AMR is a serious global health concern,” they noted.
So, what can be done to prevent it? The researchers also showed that reducing blood sugar levels in diabetic models, through the administration of insulin, deprived bacteria of their fuel, keeping their numbers at bay, and reducing the chances of antibiotic-resistant mutations from occurring. “Administering insulin to diabetic mice greatly reduced the emergence of RifR S. aureus … despite only partially restoring normal blood glucose levels,” the investigators stated. Their findings suggest that controlling blood sugar through insulin use could be key in preventing antibiotic resistance. “These data indicate that controlling diabetes with insulin helps to prevent the emergence of antibiotic-resistant S. aureus.”
Conlon added, “Resistance and its spread are not only associated with the prescription of drugs, but also the health status of those that are taking antibiotics. Controlling blood glucose then becomes really important. When we gave our mice insulin, we were able to bring their blood sugar back to normal and we didn’t get this rapid proliferation of resistant bacteria.”
The investigators are expanding their efforts to study the evolution of resistance in humans (with and without diabetes) and other antibiotic-resistant bacteria of interest, including Enterococcus faecalis, Pseudomonas aeruginosa, and Streptococcus pyogenes. Recognizing how large a role the host plays a role in the evolution of antibiotic resistance, the researchers plan to perform similar studies in patients undergoing chemotherapy and recent transplant recipients to see if those populations are also prone to antibiotic-resistant infections.