Cancer cells have seemingly endless ways to evade destruction, from suppressing the immune response to forming spheres of proteins and hijacking cells’ biological rhythms. Now, scientists identified another weapon in cancer’s arsenal: its ability to grow or shrink cells to resist treatment.
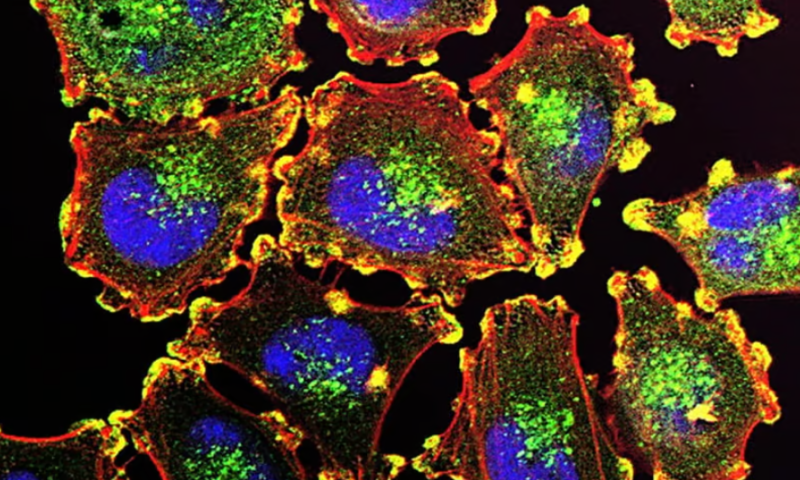
In a study published Jan. 25 in Science Advances, researchers from the Institute of Cancer Research in London described how they analyzed melanoma cells to reveal that they were capable of scaling their physical size, which corresponded to changes in gene and protein expression within the cell that could alter how well certain drugs work against them. Applying the findings to a clinical setting could help doctors determine which drugs would be best suited for a patient’s cancer, the researchers said.
“We think our research has real diagnostic potential,” Chris Bakal, Ph.D., the study’s lead author, said in a press release. “By looking at cell size, pathologists could predict whether a drug will work or if the cells will be resistant.”
The new study builds on earlier work by other teams that had identified a relationship between the size of cells and the profile of peptides they expressed, also known as their proteome. To see how this relationship might be affecting cancer cells, the Institute of Cancer Research scientists examined melanoma cells with different gene mutations—one set with a mutation in the gene BRAF, which causes 60% of melanoma cases, and another with a mutation in NRAS, responsible for another 20% to 30% of cases. They also looked at a set of NRAS-mutated cells that develop drug resistance after being treated with BRAF inhibitors like Genetech’s Zelboraf.
Image analysis showed a clear difference in the size of the cells depending on which mutation they had. The cells with the BRAF mutation were very small, while the ones bearing the NRAS mutation were much larger. The treatment-resistant cells with the NRAS mutation were even larger.
To find out what might be behind the size difference, the researchers analyzed the cells’ proteomes. They found that the small BRAF-mutated cells had many proteins responsible for DNA repair, while the NRAS-mutated cells accumulated mutations without fixing them. This caused them to swell in size.
What the different cell types did have in common was regulation of the protein CCND1, which is involved in cell growth, metabolism and differentiation. By manipulating CCND1 through its interactions with other proteins, the cells were able to control whether they grew or shrank in size.
The findings lay the groundwork for developing better treatment strategies, the researchers said. For instance, patients with a large portion of NRAS-mutated cells might not respond to treatments that work by damaging DNA, such as chemotherapy. Their many mutations could instead make them more vulnerable to the immune system, and thus more responsive to immunotherapy, which helps the immune system recognize and destroy cancer cells.
The BRAF-mutated cells, meanwhile, might be more responsive to PARP inhibitors—Immunocore’s Kimmtrak, for instance, which was approved last year for uveal melanoma. These drugs act against proteins involved in repairing DNA damage and could work well against BRAF-mutated cells when combined with chemotherapy, the researchers said. Eventually, using AI to assess the pathology of the cells could help identify which treatments would be most likely to work, Bakal added in the press release.
The scientists have already begun studying the use of immunotherapy in NRAS-mutated cells and are also investigating how growing and shrinking cancer cells play a role in breast, head and neck cancers. They hope their findings will lead to new drug development, too, such as agents that target the proteins that scale cancer cells up and down.