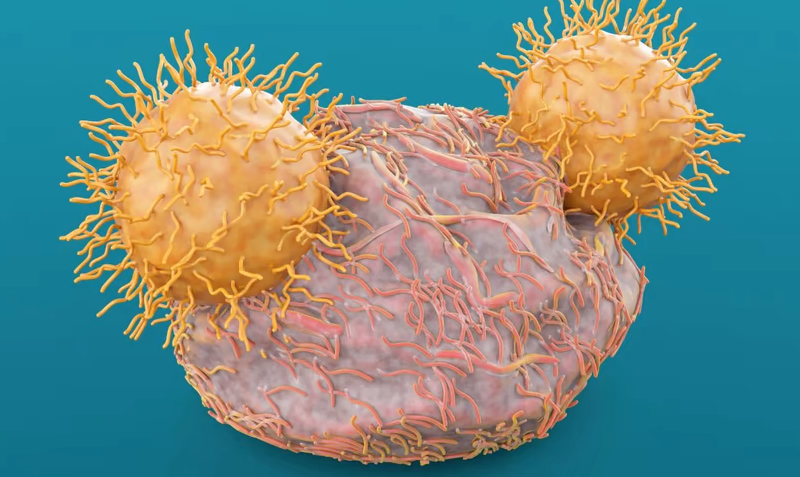
A major hurdle for using engineered CAR-T cells to treat solid tumors is the lack of tumor-specific markers for therapies to target. By leveraging a unique genetic feature that separates tumors from normal cells, scientists at A2 Biotherapeutics have designed dual-signal CAR-T cells to address the problem in solid cancers.
A2 Bio designed the Tmod T-cell therapy platform for precise tumor targeting. The system incorporates two receptors in the CAR construct, which can shut down the T cells in healthy cells.
CAR-T cells designed based on the Tmod platform killed off colorectal cancer cells expressing the carcinoembryonic antigen (CEA) protein in lab dishes and in mice without affecting normal cells, A2 Bio reported in a paper published in Science Translational Medicine. A separate CAR Tmod construct targeting mesothelin (MSLN) showed similar action against solid tumors in preclinical models, a study published in the Journal for ImmunoTherapy of Cancer showed.
A2 Bio is advancing its two lead CAR-T programs, A2B530 for CEA and A2B694 for MSLN, into human clinical trials against multiple solid tumor types.
Like other CAR-T cell products, Tmod includes an activator that can awaken T cells when exposed to a specific antigen. But antigens like CEA and MSLN are highly expressed on healthy tissues as well as various tumor cells. To specifically target tumors, A2 Bio takes advantage of a genetic phenomenon called loss of heterozygosity, in which one of the two parental genes—or alleles—at the same position on a chromosome is lost. The problem is common in tumor cells.
For the blocker module of CAR, the A2 Bio researchers chose the HLA-A*02 antigen, which is produced when both alleles are present. They linked a piece of antibody for HLA-A*02 with an immune inhibitory receptor called LIR-1. So, when encountering a healthy cell that expresses HLA-A*02 normally, the blocker would recognize it and turn off the killing effect of T cells.
The CEA Tmod cells rapidly eliminated colorectal cancer cells expressing CEA but lacked HLA-A*02 in cell culture and shrank colorectal tumors in a mouse xenograft model, with similar potency as TCR T cells, the team reported. By comparison, healthy cells expressing HLA-A*02 grew in mice treated with the CEA Tmod as they did in control animals.
The team recorded similar results for the MSLN Tmod cells in a mouse xenograft model bearing engineered cervical cancer. Both typical CAR-T cells and Tmod cells killed MSLN-expressing, A*02-negative tumor cells equally well, the team reported. But while CAR-T cells also inhibited the growth of surrogate “normal” MSLN cells that also expressed A*-02, the Tmod cells spared them.
Several T-cell therapies have been approved to treat blood cancers. The Tmod approach reflects a larger effort to direct the powerful immuno-oncology method against solid tumors by exploring ways to safeguard healthy cells.
Senti Bio, for example, is developing logic-gated CAR therapies. The company’s SENTI-401 is an allogeneic, CAR-natural killer cell therapy being developed for colorectal cancer. The experimental therapy also targets CEA but uses the membrane protein VSIG2 as a safety antigen in its inhibitory domain to steer the therapy away from healthy cells.
In the new studies, A2 Bio showed that its Tmod strategy could also be used in other types of tumor antigens and HLA alleles. Through a collaboration formed in late 2020, A2 Bio is working with Merck & Co. to develop an allogeneic Tmod cell therapy against an undisclosed target.